On May 18, 1896, the U.S. Supreme Court issued its Plessy v. Ferguson ruling, which upheld the constitutionality of racial segregation laws within the
“separate but equal” doctrine. That was the world Edna D. Kennedy had been born into
just five weeks prior. As an African American, she would face challenges in a society
that did not offer separate but equal opportunities into the medical profession. Not
only would her race limit her access to medical schools; so, too, would her gender.
Despite the odds, this native Philadelphian—known as Edna K. Williams, DO, throughout
her career—would follow in the footsteps of Meta L. Christy, DO 1921, as PCOM’s second African American alumna and a role model for the community and
other Black medical professionals.
At the turn of the 20th century, the Kennedy family resided at 625 Pine Street, then
an African American and immigrant neighborhood. Edna, the daughter of a laborer, was
the eldest of three. By 1910, the family, including one grandmother, moved into a
two-story row house in South Philadelphia. Edna attended Philadelphia High School
for Girls, followed by a practical education at the Derrick Shorthand School of Philadelphia.
Stenography was a reasonable career expectation for a Black woman of her times—and,
as it turned out, not a bad skill to have for taking notes as a medical student!
But before medical school came marriage, a baby, a divorce and another marriage, all
between 1918 and 1920. Husband Dayton H. C. Wilson, a bellman and, in later years,
a physician, spent part of their newlywed year on active duty for World War I. While
he was deployed, daughter Phylomina was born. By 1920, the estranged couple was living
a block apart—with their respective parents—and Edna Kennedy was employed as a stenographer
for a fraternal society. In August 1920, she married Alphonzo L. Williams, a chauffer
from the District of Columbia, and this time took her husband’s name.
Turpy, the treatment guru
As the 1920s roared, this wife and mother hunkered down for life as a medical student,
matriculating at PCOM’s Spring Garden Street location in 1922. Classmates came to
know her as “Turpy.” Comments published in the PCOM Synapsis yearbook hint at her drive and perseverance. In 1925: “We have naught but praises
for this young lady as she pioneers in this great science. She exhibits great pluck
in carrying on.” And, in 1926:
I see here none other than Edna Williams, hard at work over a new demonstrating machine
which enables the beginner to locate lesions by a crier which says “that’s it” or
“no, you’re wrong.” Edna has tried many models, as may be seen by looking around,
but this machine is no doubt “the” one.
At age 30, Dr. Williams graduated from PCOM, one of 18 women and the only African
American woman in her class.
Dr. Williams started a family practice in a rented three-story row house in Philadelphia’s
Brewerytown neighborhood. She also opened an office in New Jersey. She kept fees very
low, particularly to make health care affordable during the Great Depression. By 1935,
husband Alphonzo had returned to Washington. Dr. Williams and Phylomina relocated
to 219 East Upsal Street (East Mt. Airy), where she ran her family practice that included
delivering babies, sometimes in the middle of the night. Patients referred to her
as “the treatment guru.”
Although small in stature—barely five feet tall—Dr. Williams had a stool to stand
on and strong therapeutic hands to perform osteopathic manipulative treatment. Valerie Griffin, who later worked with Dr. Williams at Gemedco Medical Center in
Germantown, recalls how “She surprised a lot of the 200- to 250-pound men who came
for treatment and manipulation with the strength of her hands.”
A call to minister
While Dr. Williams healed patients physically with her hands, by 1945, she was applying
her religious convictions to minister in other ways. Dr. Williams was affiliated with
the Third Christian Scientist denomination as a lecturer and teacher. She orated about
pathways to spiritual, mental, financial and physical health by channeling God’s healing
life currents; she also discussed reincarnation. One could say she exemplified a holistic
approach to medicine. Dr. Williams established a chapel on the second floor of a brownstone
at 2307 North Broad Street, where she conducted free weekly lectures, sometimes four
times each Sunday.
By 1949, a growing following likely led Dr. Williams to relocate her chapel to 902
Walnut Street and expand her ministry to “Dr. Edna K. Williams Associates.” Her program
spread beyond Philadelphia to bases in Baltimore, New York, and Washington, DC, and
advertisements for her lectures appeared in Pittsburgh newspapers in the mid-1950s.
In her spare time, Dr. Williams enjoyed singing, which she combined with community
service. She belonged to the Western Helpers’ Club, which sang Christmas carols to
patients at the Children’s Hospital of Philadelphia. She also performed for a Germantown
flower club.
Not the retiring type
When Dr. Williams retired from private practice, she did not stay in retirement for
long. William M. King, DO ’62, who established the Gemedco Medical Center in 1976,
convinced Dr. Williams to come out of retirement to work at the community medical
center. She started off working one day a week, seeing 20 to 25 patients a day. Eventually,
she slowed down to one morning a week and five to six patients—still a remarkable
effort given that she was approaching 90.
In 1989, Dr. Williams retired for good at age 92. That same year, PCOM established
a scholarship in her name to assist minority and ethnic students. She suffered a stroke
and the loss of her daughter before passing away on September 28, 1993. Ms. Griffin
remembers Dr. Williams as
quiet and soft spoken, but firm, and a very warm and kind-hearted spirit. She was
always willing to share her knowledge of perseverance—going through medical school,
how hard it was as a woman and a woman of color. She was very much a role model, encouraging
others to keep striving and persevere.
Back to Top









 ”My first recollection of Dr. Allen wasn’t connected to PCOM, or even knowing that
she was a physician. I was born in the Philadelphia area, and my parents were always
socially conscious and politically active. Dr. Allen was held in high regard as a
politician. She was the first Black woman to serve on Philadelphia City Council, in
1971, and later she was elected to an at-large Council seat. She was a Republican,
which was a little bit different for a Black elected official in Philadelphia, then
and now. She repeatedly described herself: as ‘a BFR—a Black female Republican, an
entity as rare as a black elephant and just as smart.’ … She entered politics as a
byproduct of being a physician. She’d been interested in becoming a doctor from the
time she was a little girl. But as a Black woman, she found that her applications
to medical school met with resistance. She later championed and mentored underrepresented
minorities in medicine. The Dr. Ethel Allen Endowed Memorial Scholarship at PCOM continues
to support Black women students. … Dr. Allen treated patients in some of the most
underserved communities in Philadelphia, and the socio-economic issues seen in many
of these communities are what spurred her to run for elected office. … Her name came
up in the Philadelphia press just recently. A Democrat, Rue Landau, won one of five
nominations for at-large seats on the Council, and if elected in November she’ll become
the first openly LGBTQ City Council member. The Philadelphia Inquirer said, ‘In her victory speech, Landau paid homage to at least two gay Council members
who were not out during their political tenure.’ One of them was Dr. Allen. … In 1976,
after Governor Milton Shapp had issued an executive order to create the Pennsylvania
Council for Sexual Minorities, Dr. Allen successfully lobbied for him to issue a proclamation
in support of Gay Pride Week. And in 1979, when Governor Dick Thornburgh appointed
her Secretary of the Commonwealth of Pennsylvania, she became the highest-ranking
Black woman in the state, and was responsible for Thornburgh declaring June to be
Gay Pride Month in Pennsylvania. … Dr. Allen was a trailblazer: before her time, and
looking to serve. She deserves more recognition for her efforts to lift up impoverished
people, to improve the health outcomes of underserved communities, and to champion
the rights of those who lacked them.”
”My first recollection of Dr. Allen wasn’t connected to PCOM, or even knowing that
she was a physician. I was born in the Philadelphia area, and my parents were always
socially conscious and politically active. Dr. Allen was held in high regard as a
politician. She was the first Black woman to serve on Philadelphia City Council, in
1971, and later she was elected to an at-large Council seat. She was a Republican,
which was a little bit different for a Black elected official in Philadelphia, then
and now. She repeatedly described herself: as ‘a BFR—a Black female Republican, an
entity as rare as a black elephant and just as smart.’ … She entered politics as a
byproduct of being a physician. She’d been interested in becoming a doctor from the
time she was a little girl. But as a Black woman, she found that her applications
to medical school met with resistance. She later championed and mentored underrepresented
minorities in medicine. The Dr. Ethel Allen Endowed Memorial Scholarship at PCOM continues
to support Black women students. … Dr. Allen treated patients in some of the most
underserved communities in Philadelphia, and the socio-economic issues seen in many
of these communities are what spurred her to run for elected office. … Her name came
up in the Philadelphia press just recently. A Democrat, Rue Landau, won one of five
nominations for at-large seats on the Council, and if elected in November she’ll become
the first openly LGBTQ City Council member. The Philadelphia Inquirer said, ‘In her victory speech, Landau paid homage to at least two gay Council members
who were not out during their political tenure.’ One of them was Dr. Allen. … In 1976,
after Governor Milton Shapp had issued an executive order to create the Pennsylvania
Council for Sexual Minorities, Dr. Allen successfully lobbied for him to issue a proclamation
in support of Gay Pride Week. And in 1979, when Governor Dick Thornburgh appointed
her Secretary of the Commonwealth of Pennsylvania, she became the highest-ranking
Black woman in the state, and was responsible for Thornburgh declaring June to be
Gay Pride Month in Pennsylvania. … Dr. Allen was a trailblazer: before her time, and
looking to serve. She deserves more recognition for her efforts to lift up impoverished
people, to improve the health outcomes of underserved communities, and to champion
the rights of those who lacked them.” ”I met Charbel on my first day at PCOM. He and I soon realized we had graduated from
the same school, Georgia State University, and even the same program. And his nonprofit,
the Georgia First Generation Foundation, is near and dear to my heart, because that’s
my research interest. That’s how our friendship/mentorship blossomed. … The foundation
started in 2016 as a student club when Charbel was an undergraduate. He is the first
in his family to go to college, and he wanted to find ways to help other first gen
students. He got a grant to form the foundation, and now it’s one of PCOM’s community
partners in Suwanee. Valerie Cadet, assistant dean of health equity integration, PCOM
Georgia; Michael Feng, DO ‘23; and Diana Tran, PharmD ‘21, serve on the board. The
foundation is devoted to providing resources for first generation students who are
passionate about achieving academic success after high school. There’s a focus on
Gwinnett County schools. … Students are introduced to the industry’s best in various
fields, with keynote speakers at an annual summit, student and career panels, and
scholarship presentations. Success, Service and Scholarship are the organization’s
three pillars. … Charbel has two master’s degrees from PCOM, and now he’s in a doctoral
program, and on top of that he’s a director of a nonprofit. But he’s always offering
to volunteer, to step in whenever I need him. ‘Charbel, I need a healthcare student
panel. Can you serve on it?’ ‘Sure, I can do that.’ A month after I started in my
position, I had to help a middle school with their STEM certification. ‘Charbel, are
you available?’ ‘Of course, I can do that.’ … So many of our students want to do community
work and want to be involved at so many levels. They have that same drive and determination
that Charbel has. … I’ve heard Charbel speak about the ways in which his Lebanese
cultural identity has an impact on how he works and how he presents himself on campus.
First gen students are a diverse group, very proud of their backgrounds. Some are
the first in their families to be formally educated in this country. My overarching
goal is to make sure I support my students in whatever they want to do, whatever goals
they have.”
”I met Charbel on my first day at PCOM. He and I soon realized we had graduated from
the same school, Georgia State University, and even the same program. And his nonprofit,
the Georgia First Generation Foundation, is near and dear to my heart, because that’s
my research interest. That’s how our friendship/mentorship blossomed. … The foundation
started in 2016 as a student club when Charbel was an undergraduate. He is the first
in his family to go to college, and he wanted to find ways to help other first gen
students. He got a grant to form the foundation, and now it’s one of PCOM’s community
partners in Suwanee. Valerie Cadet, assistant dean of health equity integration, PCOM
Georgia; Michael Feng, DO ‘23; and Diana Tran, PharmD ‘21, serve on the board. The
foundation is devoted to providing resources for first generation students who are
passionate about achieving academic success after high school. There’s a focus on
Gwinnett County schools. … Students are introduced to the industry’s best in various
fields, with keynote speakers at an annual summit, student and career panels, and
scholarship presentations. Success, Service and Scholarship are the organization’s
three pillars. … Charbel has two master’s degrees from PCOM, and now he’s in a doctoral
program, and on top of that he’s a director of a nonprofit. But he’s always offering
to volunteer, to step in whenever I need him. ‘Charbel, I need a healthcare student
panel. Can you serve on it?’ ‘Sure, I can do that.’ A month after I started in my
position, I had to help a middle school with their STEM certification. ‘Charbel, are
you available?’ ‘Of course, I can do that.’ … So many of our students want to do community
work and want to be involved at so many levels. They have that same drive and determination
that Charbel has. … I’ve heard Charbel speak about the ways in which his Lebanese
cultural identity has an impact on how he works and how he presents himself on campus.
First gen students are a diverse group, very proud of their backgrounds. Some are
the first in their families to be formally educated in this country. My overarching
goal is to make sure I support my students in whatever they want to do, whatever goals
they have.” ”During my internship at Metropolitan Hospital Central Division, I fell in love with
critical care and procedural-based medicine. I reached out to
”During my internship at Metropolitan Hospital Central Division, I fell in love with
critical care and procedural-based medicine. I reached out to  “When I first met Nicole, she stood out as if there was a spotlight on her; you just
knew early on that she was going to go further in her career, beyond being a great
physician. The way she spoke, the way she carried herself—there was always a memory
of something about her, something she said, that you took with you when you left the
room. Within the
“When I first met Nicole, she stood out as if there was a spotlight on her; you just
knew early on that she was going to go further in her career, beyond being a great
physician. The way she spoke, the way she carried herself—there was always a memory
of something about her, something she said, that you took with you when you left the
room. Within the  ”Jim and I were PCOM classmates. He completed an internship at the Fort Worth Osteopathic
Hospital and then an anesthesiology residency. He practiced in Fort Worth for more
than 10 years until he decided to join the Navy and became a flight surgeon [assigned
to the USS Ranger (CV-61)] … Jim is a very private and unassuming person who will not tell you that
he retired after many years with the rank of Rear Admiral; that he was Fleet Surgeon
for both the Pacific and Atlantic Fleets; that he was Commanding Officer of the Naval
Hospital in Oak Harbor, Washington, and of the Naval Hospital in Yokosuka, Japan;
that he was Medical Advisor to the Supreme Allied Commander Atlantic, which is the
NATO Command. He was the third DO to achieve flag status in the Navy. I learned all
this when we became reacquainted when he moved to Broward County to be close to his
elderly mother. … My wife, Lila, and I were fond of cruising to many countries, and
Jim and his wife, Joann, were wonderful companions to us and to our son and his family.
Jim was like an uncle to our grandchildren during our shared visits to Colorado every
summer. … One of Jim’s exciting stories—I recall having dragged it out of him—was
when he was lowered from a helicopter to a surfaced submarine to examine a seaman
who had appendicitis. There must be more such stories that I haven’t heard yet. …
Jim is an active member of the Board of the Navy League of Fort Lauderdale, which
supports visiting ships and their crews as well as providing a social and educational
platform for retired members of the Navy and Marines. He even got me to join as a
supporting member. … Jim is a man of impeccable ethics and faith and is a
”Jim and I were PCOM classmates. He completed an internship at the Fort Worth Osteopathic
Hospital and then an anesthesiology residency. He practiced in Fort Worth for more
than 10 years until he decided to join the Navy and became a flight surgeon [assigned
to the USS Ranger (CV-61)] … Jim is a very private and unassuming person who will not tell you that
he retired after many years with the rank of Rear Admiral; that he was Fleet Surgeon
for both the Pacific and Atlantic Fleets; that he was Commanding Officer of the Naval
Hospital in Oak Harbor, Washington, and of the Naval Hospital in Yokosuka, Japan;
that he was Medical Advisor to the Supreme Allied Commander Atlantic, which is the
NATO Command. He was the third DO to achieve flag status in the Navy. I learned all
this when we became reacquainted when he moved to Broward County to be close to his
elderly mother. … My wife, Lila, and I were fond of cruising to many countries, and
Jim and his wife, Joann, were wonderful companions to us and to our son and his family.
Jim was like an uncle to our grandchildren during our shared visits to Colorado every
summer. … One of Jim’s exciting stories—I recall having dragged it out of him—was
when he was lowered from a helicopter to a surfaced submarine to examine a seaman
who had appendicitis. There must be more such stories that I haven’t heard yet. …
Jim is an active member of the Board of the Navy League of Fort Lauderdale, which
supports visiting ships and their crews as well as providing a social and educational
platform for retired members of the Navy and Marines. He even got me to join as a
supporting member. … Jim is a man of impeccable ethics and faith and is a  ”I got to know Dr. Blanck as a
”I got to know Dr. Blanck as a  ”I met Dr. Bullock in 1988 when I started medical school at PCOM, at a time when there
were not many physicians or faculty members of color, at a time when diversity and
inclusion were not topics of open discussion. Since there were only a few students
of color at PCOM, we naturally gravitated to Dr. Bullock. He served as our role model
and mentor. Dr. Bullock took us under his wing, nurturing us and making sure we had
the resources and encouragement needed to succeed. … I often reached out to him for
guidance. I requested to work with him at
”I met Dr. Bullock in 1988 when I started medical school at PCOM, at a time when there
were not many physicians or faculty members of color, at a time when diversity and
inclusion were not topics of open discussion. Since there were only a few students
of color at PCOM, we naturally gravitated to Dr. Bullock. He served as our role model
and mentor. Dr. Bullock took us under his wing, nurturing us and making sure we had
the resources and encouragement needed to succeed. … I often reached out to him for
guidance. I requested to work with him at  ”Dr. Cathie knew anatomy about as well as any person could, and he taught anatomy
about as well as anyone possibly could. He had a distinct love of the profession of
osteopathic medicine. … He also had the unbelievable ability to draw anatomic pictures
on the blackboard, using multiple colors, with both hands at the same time—while he
was also lecturing. … You did hope you would not be called on to participate in a
discussion for which you probably would not have the full knowledge he expected. So
people were somewhat reticent and would slink back in their chairs during his lectures.
… In those days, a group of four or five students worked together on one body. Dr.
Cathie would move diligently from table to table, reviewing the anatomy, correcting
our impressions, helping in our dissections. He was absolutely superb in that respect.
… On the other hand, I recall one situation very early in our program when we were
doing the dissection, and he was at the front of the class having lunch. That hit
some people in a strange way, and a few had to leave the room. … In the second semester
of our junior year, Dr. Cathie taught a class in
”Dr. Cathie knew anatomy about as well as any person could, and he taught anatomy
about as well as anyone possibly could. He had a distinct love of the profession of
osteopathic medicine. … He also had the unbelievable ability to draw anatomic pictures
on the blackboard, using multiple colors, with both hands at the same time—while he
was also lecturing. … You did hope you would not be called on to participate in a
discussion for which you probably would not have the full knowledge he expected. So
people were somewhat reticent and would slink back in their chairs during his lectures.
… In those days, a group of four or five students worked together on one body. Dr.
Cathie would move diligently from table to table, reviewing the anatomy, correcting
our impressions, helping in our dissections. He was absolutely superb in that respect.
… On the other hand, I recall one situation very early in our program when we were
doing the dissection, and he was at the front of the class having lunch. That hit
some people in a strange way, and a few had to leave the room. … In the second semester
of our junior year, Dr. Cathie taught a class in  ”Dr. Cathie [at the time, Dr. Waddel] was an excellent teacher and a very hard taskmaster
who wanted her students to understand the pathology of the diseases they were going
to be seeing in clinical practice. When you first met her in the classroom, you were
scared to death of her. I can remember pulling all-nighters just to pass her exams.
But when you got to really know her, she was a cupcake. … She wasn’t only a good teacher;
she was a good student as well. She’s probably among the first women to be certified
in cytopathology, studying under Papanicolaou himself. I asked her to teach me how
to do Pap smears, and spent many afternoons after class with her learning how to read
them. … I also had the opportunity to see her on a more personal basis. A few of us
women students wanted to form a chapter of Delta Omega, one of the female medical
sororities on the campuses of the other medical schools in town. We needed a mentor,
and she very graciously and very enthusiastically agreed to take on that role. We
had our meetings at her home, where she provided both professional and personal guidance.
Some of it dealt with how we were looked upon as women in the profession—good advice
in terms of just being who you are and doing what you have to do. She was the first
woman to chair a basic science department at PCOM [and at that time, the only woman—other
than those at Women’s Medical College—who held such a position in the entire City
of Philadelphia]. … Dr. Cathie suggested that I take a career in pathology. But I
really didn’t like the idea of doing a lot of autopsies, and at that time they did
a heck of a lot more than we do today. But after about eight years in general practice,
I decided to go into something with a lifestyle that was more in line with raising
a family at the same time. And I chose pathology and laboratory medicine, which led
me to teaching positions and three directorships of hospital laboratories. … Years
after Dr. Cathie had retired, I met her at one of the American Osteopathic Association
conventions. She congratulated me on my achievements, and I told her that I had some
truly big footsteps to follow in.”
”Dr. Cathie [at the time, Dr. Waddel] was an excellent teacher and a very hard taskmaster
who wanted her students to understand the pathology of the diseases they were going
to be seeing in clinical practice. When you first met her in the classroom, you were
scared to death of her. I can remember pulling all-nighters just to pass her exams.
But when you got to really know her, she was a cupcake. … She wasn’t only a good teacher;
she was a good student as well. She’s probably among the first women to be certified
in cytopathology, studying under Papanicolaou himself. I asked her to teach me how
to do Pap smears, and spent many afternoons after class with her learning how to read
them. … I also had the opportunity to see her on a more personal basis. A few of us
women students wanted to form a chapter of Delta Omega, one of the female medical
sororities on the campuses of the other medical schools in town. We needed a mentor,
and she very graciously and very enthusiastically agreed to take on that role. We
had our meetings at her home, where she provided both professional and personal guidance.
Some of it dealt with how we were looked upon as women in the profession—good advice
in terms of just being who you are and doing what you have to do. She was the first
woman to chair a basic science department at PCOM [and at that time, the only woman—other
than those at Women’s Medical College—who held such a position in the entire City
of Philadelphia]. … Dr. Cathie suggested that I take a career in pathology. But I
really didn’t like the idea of doing a lot of autopsies, and at that time they did
a heck of a lot more than we do today. But after about eight years in general practice,
I decided to go into something with a lifestyle that was more in line with raising
a family at the same time. And I chose pathology and laboratory medicine, which led
me to teaching positions and three directorships of hospital laboratories. … Years
after Dr. Cathie had retired, I met her at one of the American Osteopathic Association
conventions. She congratulated me on my achievements, and I told her that I had some
truly big footsteps to follow in.” ”John joined PCOM full time shortly after I did in 1999. He became the
”John joined PCOM full time shortly after I did in 1999. He became the  “I worked for Gene from 1994 to 2019. I was the CFO of his business, Almo Corporation;
he was the chairman and the CEO at the time that I joined. He’s a very collaborative
leader who solicits input from all of his folks, not just his management team. And
as a mentor he was always willing to share his knowledge and experience with me as
well as with others. He’s open, approachable, personable. That’s an extremely effective
management style. … When I was interviewing for the job with Gene, he gave me a tour
of one of his warehouse facilities, and as we walked through, an employee greeted
us. I was struck by the fact that he and Gene called each other by their first names.
That told me an awful lot about Gene and the inclusive culture he had created. I had
come out of primarily large corporate public companies—buttoned up, maybe a little
stiff. I went through a period of adjustment, but obviously it worked out. … Gene
always spoke highly of PCOM, and he really enjoyed his 24 years as a trustee, 23 years
spent as vice chairman. Around 2013, he asked me if I had an interest in joining the
Board, and that’s how I got to be where I am. … Gene is loyal to the causes that drive
him, and he wants to leave the world in a better place. I think his motivations are
compelling and simple and earnest. He has a keen interest in the lives of the people
that he’s talking to. That is a consistent feature of being around Gene. He does not
make the conversation about himself, despite his successes and his station in this
world. He’s understated and warm. … In addition to his financial expertise, Gene is
a very good decision maker and has always had a strong interest in supporting programs
that help the students at PCOM. He’s a pretty darn good role model for anybody in
the business community who would aspire to lend their talents to worthy organizations
or institutions.”
“I worked for Gene from 1994 to 2019. I was the CFO of his business, Almo Corporation;
he was the chairman and the CEO at the time that I joined. He’s a very collaborative
leader who solicits input from all of his folks, not just his management team. And
as a mentor he was always willing to share his knowledge and experience with me as
well as with others. He’s open, approachable, personable. That’s an extremely effective
management style. … When I was interviewing for the job with Gene, he gave me a tour
of one of his warehouse facilities, and as we walked through, an employee greeted
us. I was struck by the fact that he and Gene called each other by their first names.
That told me an awful lot about Gene and the inclusive culture he had created. I had
come out of primarily large corporate public companies—buttoned up, maybe a little
stiff. I went through a period of adjustment, but obviously it worked out. … Gene
always spoke highly of PCOM, and he really enjoyed his 24 years as a trustee, 23 years
spent as vice chairman. Around 2013, he asked me if I had an interest in joining the
Board, and that’s how I got to be where I am. … Gene is loyal to the causes that drive
him, and he wants to leave the world in a better place. I think his motivations are
compelling and simple and earnest. He has a keen interest in the lives of the people
that he’s talking to. That is a consistent feature of being around Gene. He does not
make the conversation about himself, despite his successes and his station in this
world. He’s understated and warm. … In addition to his financial expertise, Gene is
a very good decision maker and has always had a strong interest in supporting programs
that help the students at PCOM. He’s a pretty darn good role model for anybody in
the business community who would aspire to lend their talents to worthy organizations
or institutions.” ”I come from a family of immigrants, and I’m the first in my family to attend medical
school. So for me to know
”I come from a family of immigrants, and I’m the first in my family to attend medical
school. So for me to know  ”When I first applied for admission to PCOM, Dr. Cipolla was a member of the interview
committee. He asked me only one question: ‘Do you know who invented spaghetti?’ And
I said, ‘No.’ ‘Well,’ he told me, ‘the Chinese actually invented spaghetti, not the
Italians.’ And that was the extent of our interaction. … The next time I saw him was
in the fall of 1977, in my first anatomy lecture held in Evans Hall (now known as
the Howard A. Hassman, DO ’83 Academic Center). His opening line was, ‘You gotta know
your anatomy, boy, or the guy down the street will.’… The anatomy lab was at 48th
and Spruce Streets, where the old hospital used to be. The anatomy lab was almost
like an attic, with the smell of formaldehyde everywhere. It had a great feel to it.
… You had to wear a tie, which on the surface seems absurd. But I think in part the
reason was Dr. Cipolla’s profound respect for the people who had donated their bodies
to medical science. In my kind of rebellious way, I would wear a flannel shirt with
a tie. One day, early on, Dr. Cipolla just kind of looked at me and grinned, and then
that was it. … In anatomy lab, you have partners, you’d be helping each other out.
And every once in a while, I’d turn around and, over my shoulder, he’d be there, listening.
… I loved anatomy. I would often go down to the lab on Saturdays. Dr. Cipolla asked
me one day, ‘Why are you here all the time?’ I said, ‘It’s a chance to have the cadaver
all to myself. I don’t have to share it with my lab partners.’ He got a kick out of
that. … Over the course of time, he’d walk around during lab, and he’d ask one table
an anatomy question, and if they didn’t get it, he’d say, ‘Hey, Feldstein. You know
the answer.’ So we had this mutual respect, an intellectual understanding. … He was
a general surgeon in the Medical Corp and he would throw in tidbits, with clinical
correlation, during anatomy lectures—practical examples of what you were learning.
… He could be difficult; he was as eccentric as they come—definitely the type of individual
you either loved or hated. Had I struggled in anatomy, it might not have been as much
fun. But he was brilliant.”
”When I first applied for admission to PCOM, Dr. Cipolla was a member of the interview
committee. He asked me only one question: ‘Do you know who invented spaghetti?’ And
I said, ‘No.’ ‘Well,’ he told me, ‘the Chinese actually invented spaghetti, not the
Italians.’ And that was the extent of our interaction. … The next time I saw him was
in the fall of 1977, in my first anatomy lecture held in Evans Hall (now known as
the Howard A. Hassman, DO ’83 Academic Center). His opening line was, ‘You gotta know
your anatomy, boy, or the guy down the street will.’… The anatomy lab was at 48th
and Spruce Streets, where the old hospital used to be. The anatomy lab was almost
like an attic, with the smell of formaldehyde everywhere. It had a great feel to it.
… You had to wear a tie, which on the surface seems absurd. But I think in part the
reason was Dr. Cipolla’s profound respect for the people who had donated their bodies
to medical science. In my kind of rebellious way, I would wear a flannel shirt with
a tie. One day, early on, Dr. Cipolla just kind of looked at me and grinned, and then
that was it. … In anatomy lab, you have partners, you’d be helping each other out.
And every once in a while, I’d turn around and, over my shoulder, he’d be there, listening.
… I loved anatomy. I would often go down to the lab on Saturdays. Dr. Cipolla asked
me one day, ‘Why are you here all the time?’ I said, ‘It’s a chance to have the cadaver
all to myself. I don’t have to share it with my lab partners.’ He got a kick out of
that. … Over the course of time, he’d walk around during lab, and he’d ask one table
an anatomy question, and if they didn’t get it, he’d say, ‘Hey, Feldstein. You know
the answer.’ So we had this mutual respect, an intellectual understanding. … He was
a general surgeon in the Medical Corp and he would throw in tidbits, with clinical
correlation, during anatomy lectures—practical examples of what you were learning.
… He could be difficult; he was as eccentric as they come—definitely the type of individual
you either loved or hated. Had I struggled in anatomy, it might not have been as much
fun. But he was brilliant.” ”Managing Emotional Systems in the Workplace was my first class, Bill Clinton’s last
before his retirement in 2017. As a busy working woman going back to school in her
forties, I was excited to start my master’s degree program in Organizational Development
and Leadership [ODL]. Little did I know how deeply my first grad school course with
Bill would impact my life. … First class, an all-day Saturday session, Bill handed
each of us a lengthy paper he’d written on the 10 most impactful incidents in his
life, including some traumatic episodes. As I read his deeply personal passages, I
thought, ‘Wow, this guy is really putting himself out here.’ … Our first assignment
was to lay bare our souls, to do the same sort of self-reflection as Bill had done
in his raw and revealing autobiography by chronicling what we could have done differently
to better our career and our relationships with our family and friends. … Bill felt
emotional transparency was the key to building trust with your colleagues and to being
a strong workplace leader. His mantra: ‘I want you to know who I am and to trust who
I am so that you can be transparent with me.’ He taught that you can only achieve
that level of openness by understanding others’ points of view, which often meant
having difficult conversations and finding closure with those with whom you’d had
thorny relationships. … It was risky, but the reward of growing into a more empathetic
and understanding person made it all worthwhile. Bill taught me to appreciate the
person and the personality, not just the work product, because who you are affects
everything about you in the workplace. … Fast forward three years to my capstone project,
which focused on my transformative story of personal growth that I rough-drafted in
that first grad-school paper. I presented my capstone virtually due to the pandemic.
Whose warm and welcoming face did I see smiling back at me on the Zoom meeting? Bill
Clinton’s. I was so moved and honored that he was present and that I was one of the
last students he taught in his 15 years as director of the College’s ODL program.”
”Managing Emotional Systems in the Workplace was my first class, Bill Clinton’s last
before his retirement in 2017. As a busy working woman going back to school in her
forties, I was excited to start my master’s degree program in Organizational Development
and Leadership [ODL]. Little did I know how deeply my first grad school course with
Bill would impact my life. … First class, an all-day Saturday session, Bill handed
each of us a lengthy paper he’d written on the 10 most impactful incidents in his
life, including some traumatic episodes. As I read his deeply personal passages, I
thought, ‘Wow, this guy is really putting himself out here.’ … Our first assignment
was to lay bare our souls, to do the same sort of self-reflection as Bill had done
in his raw and revealing autobiography by chronicling what we could have done differently
to better our career and our relationships with our family and friends. … Bill felt
emotional transparency was the key to building trust with your colleagues and to being
a strong workplace leader. His mantra: ‘I want you to know who I am and to trust who
I am so that you can be transparent with me.’ He taught that you can only achieve
that level of openness by understanding others’ points of view, which often meant
having difficult conversations and finding closure with those with whom you’d had
thorny relationships. … It was risky, but the reward of growing into a more empathetic
and understanding person made it all worthwhile. Bill taught me to appreciate the
person and the personality, not just the work product, because who you are affects
everything about you in the workplace. … Fast forward three years to my capstone project,
which focused on my transformative story of personal growth that I rough-drafted in
that first grad-school paper. I presented my capstone virtually due to the pandemic.
Whose warm and welcoming face did I see smiling back at me on the Zoom meeting? Bill
Clinton’s. I was so moved and honored that he was present and that I was one of the
last students he taught in his 15 years as director of the College’s ODL program.” ”Bob is one of the most well-rounded people I’ve ever met, and probably the smartest.
He has great intellect; he’s a fabulous writer; he has great analytical skills and
a knack for separating the wheat from the chaff. He is truly quite remarkable—one
in a million, to my mind. … In all the years I worked with Bob—and believe me, we
dealt with all kinds of issues—I never saw a bead of sweat on his brow. Absolutely
nothing made him nervous—pure grit! He knew what he needed to know. He did what he
needed to do, and he did it extremely well. He was a great source of mentorship and
consultation to me and my staff. We could go to Bob with just about any concerns.
… Bob expertly guided us and PCOM through
”Bob is one of the most well-rounded people I’ve ever met, and probably the smartest.
He has great intellect; he’s a fabulous writer; he has great analytical skills and
a knack for separating the wheat from the chaff. He is truly quite remarkable—one
in a million, to my mind. … In all the years I worked with Bob—and believe me, we
dealt with all kinds of issues—I never saw a bead of sweat on his brow. Absolutely
nothing made him nervous—pure grit! He knew what he needed to know. He did what he
needed to do, and he did it extremely well. He was a great source of mentorship and
consultation to me and my staff. We could go to Bob with just about any concerns.
… Bob expertly guided us and PCOM through  ”Al was an extraordinary man. He was certified in cardiology, but in the 1960s, when
he was just starting out, he would lecture when other professors didn’t show up. On
any topic, no notes, no preparation—off the top of his head. That’s how smart he was.
… He was drafted by the Chicago White Sox and played professional baseball up to the
double-A level. He had also played four years of varsity baseball at Duke, where he
was an honorary All American. He was a tremendous golfer. … He decided to be a doctor
like his brother and his father, and went on to be president of the American College
of Osteopathic Internists, president of the Pennsylvania Osteopathic Medical Association,
vice chairman of the
”Al was an extraordinary man. He was certified in cardiology, but in the 1960s, when
he was just starting out, he would lecture when other professors didn’t show up. On
any topic, no notes, no preparation—off the top of his head. That’s how smart he was.
… He was drafted by the Chicago White Sox and played professional baseball up to the
double-A level. He had also played four years of varsity baseball at Duke, where he
was an honorary All American. He was a tremendous golfer. … He decided to be a doctor
like his brother and his father, and went on to be president of the American College
of Osteopathic Internists, president of the Pennsylvania Osteopathic Medical Association,
vice chairman of the  ”I’ve known Joe since we were in college together at LaSalle, where we matriculated
in 1961 and were both members of the swim team for four years. In 1966, Joe and I
were both accepted to Philadelphia College of Osteopathic Medicine, and were roommates
for the first year. We both interned at what was then the Flint Osteopathic Hospital.
After his residency, Joe joined the PCOM faculty in the
”I’ve known Joe since we were in college together at LaSalle, where we matriculated
in 1961 and were both members of the swim team for four years. In 1966, Joe and I
were both accepted to Philadelphia College of Osteopathic Medicine, and were roommates
for the first year. We both interned at what was then the Flint Osteopathic Hospital.
After his residency, Joe joined the PCOM faculty in the  ”I got to know
”I got to know  ”Dr. Evans is a military man, and can be very stern. He expects things to be done
in a certain way. If I said, ‘I have an idea, and this is what I want to do,’ he would
tell me, ‘Well, Patience, if it works, you get the glory. But if it doesn’t, you get
the blame.’ I was comfortable with that; it makes you think twice and consider all
the angles. … At
”Dr. Evans is a military man, and can be very stern. He expects things to be done
in a certain way. If I said, ‘I have an idea, and this is what I want to do,’ he would
tell me, ‘Well, Patience, if it works, you get the glory. But if it doesn’t, you get
the blame.’ I was comfortable with that; it makes you think twice and consider all
the angles. … At  ”For years, Uncle Manny addressed the new DO class with his lecture on physician compassion
during the White Coat Ceremony. With his piercing blue eyes, bushy goatee and booming
voice, he resembled a majestic king from ancient times when he pointed to the lecture
hall door and proclaimed, ‘All of you who cross this threshold who do not have empathy
and compassion in your hearts, there is the door.’ … Uncle Manny, as Dr. Fliegelman
was affectionately known to hundreds of PCOM students, then shared with his fresh-faced
congregation his famous Ten C’s for being a physician who puts the patient before
all else: compassion, contact, creativity, completion, communication, competence,
caring, consideration, concern and confidence. Each C was followed by a sentence of
explanation. Compassion: Put yourself in their shoes, you have no idea what they’re
dealing with out there in the world outside of your office. Contact: A gentle pat
on the back, a warm embrace is undeniably healthy. A framed copy of the piece of notebook
paper on which I feverishly jotted down the Ten C’s some 30 years ago still hangs
in my office. … I tell friends that Uncle Manny taught me all I needed to know on
my very first day of medical school, most notably that love is the strongest medicine
(which not coincidentally is the title of my own book). He became my mentor and my
friend. He guided me through the tough times and the long hours during our many heart-to-hearts
in his Rowland Hall office. I’m forever proud to be the first recipient of the Dr.
Emanuel Fliegelman Humanitarian Award for the doctor exhibiting highly compassionate
care during residency. … Uncle Manny was a professor of
”For years, Uncle Manny addressed the new DO class with his lecture on physician compassion
during the White Coat Ceremony. With his piercing blue eyes, bushy goatee and booming
voice, he resembled a majestic king from ancient times when he pointed to the lecture
hall door and proclaimed, ‘All of you who cross this threshold who do not have empathy
and compassion in your hearts, there is the door.’ … Uncle Manny, as Dr. Fliegelman
was affectionately known to hundreds of PCOM students, then shared with his fresh-faced
congregation his famous Ten C’s for being a physician who puts the patient before
all else: compassion, contact, creativity, completion, communication, competence,
caring, consideration, concern and confidence. Each C was followed by a sentence of
explanation. Compassion: Put yourself in their shoes, you have no idea what they’re
dealing with out there in the world outside of your office. Contact: A gentle pat
on the back, a warm embrace is undeniably healthy. A framed copy of the piece of notebook
paper on which I feverishly jotted down the Ten C’s some 30 years ago still hangs
in my office. … I tell friends that Uncle Manny taught me all I needed to know on
my very first day of medical school, most notably that love is the strongest medicine
(which not coincidentally is the title of my own book). He became my mentor and my
friend. He guided me through the tough times and the long hours during our many heart-to-hearts
in his Rowland Hall office. I’m forever proud to be the first recipient of the Dr.
Emanuel Fliegelman Humanitarian Award for the doctor exhibiting highly compassionate
care during residency. … Uncle Manny was a professor of  ”Les is pure energy. He probably popped out of his mother inventing something, and
he has not stopped. We were classmates at PCOM, and because of the alphabet—Finkelstein,
Folio—I think we shared a cadaver in Anatomy lab. … It was very apparent that when
Les was a medical student, his brain was constantly on fire. He never stopped thinking
and doing. He was truly a force of nature. … He’s a retired colonel—he was a radiologist
and flight surgeon in the Air Force. Until recently he worked for the National Institutes
of Health. Now he’s at the Moffitt Cancer Center in Tampa. The guy could never retire;
he’s just got so many years ahead of him to make a difference. … Les found a role
for himself to be able to use his talents in innovation and technology as an interventional
radiologist and a cancer radiologist. For people like Les,
”Les is pure energy. He probably popped out of his mother inventing something, and
he has not stopped. We were classmates at PCOM, and because of the alphabet—Finkelstein,
Folio—I think we shared a cadaver in Anatomy lab. … It was very apparent that when
Les was a medical student, his brain was constantly on fire. He never stopped thinking
and doing. He was truly a force of nature. … He’s a retired colonel—he was a radiologist
and flight surgeon in the Air Force. Until recently he worked for the National Institutes
of Health. Now he’s at the Moffitt Cancer Center in Tampa. The guy could never retire;
he’s just got so many years ahead of him to make a difference. … Les found a role
for himself to be able to use his talents in innovation and technology as an interventional
radiologist and a cancer radiologist. For people like Les,  ”When Carol started working at PCOM, it was a much smaller place. But even three years
ago, when I left, the feeling of family remained, and through her years at PCOM, Carol
always embraced that. She really thought of everybody working there as family and
friends. … Some have wondered how those like Carol and me could have such a long tenure
in a single institution, but PCOM was constantly changing, and that made it all exciting.
Change is the lifeblood of an institution of higher education, and PCOM was very alive
through all those years. … In admissions and student affairs, Carol and I spent a
lot of time screening applicants and talking about what we wanted our classes to look
like. Carol saw every class as the future of osteopathic medicine. … Today, just about
every professional and graduate school is talking about
”When Carol started working at PCOM, it was a much smaller place. But even three years
ago, when I left, the feeling of family remained, and through her years at PCOM, Carol
always embraced that. She really thought of everybody working there as family and
friends. … Some have wondered how those like Carol and me could have such a long tenure
in a single institution, but PCOM was constantly changing, and that made it all exciting.
Change is the lifeblood of an institution of higher education, and PCOM was very alive
through all those years. … In admissions and student affairs, Carol and I spent a
lot of time screening applicants and talking about what we wanted our classes to look
like. Carol saw every class as the future of osteopathic medicine. … Today, just about
every professional and graduate school is talking about  ”Art was one of the most charismatic men I’ve ever met. There was such a charm about
him. He was a brilliant psychologist and innovative administrator. He loved to teach.
He taught through stories. You learned so much by listening to him. … He had high
expectations for everybody, and he strived to help others meet those expectations.
He was supportive, and he motivated his faculty to achieve more. For example, he required
us to become board certified at a time when only 10 percent of
”Art was one of the most charismatic men I’ve ever met. There was such a charm about
him. He was a brilliant psychologist and innovative administrator. He loved to teach.
He taught through stories. You learned so much by listening to him. … He had high
expectations for everybody, and he strived to help others meet those expectations.
He was supportive, and he motivated his faculty to achieve more. For example, he required
us to become board certified at a time when only 10 percent of  ”I’ve been at the
”I’ve been at the  ”Soon after I came to PCOM in 1989, I was asked to serve on a committee to revise
the faculty handbook and develop a tenure policy. Charlotte Greene was the chair of
the committee, which also included Michael Venditto, DO [now professor and chair,
Division of Pulmonary and Critical Care Medicine]. We had a big job to do. … Charlotte
was very knowledgeable about the multiple roles of faculty in an academic environment.
I enjoyed watching her pause for reflection, and if she didn’t have an immediate response,
she’d dig for information and come back to the table with advice for us. She worked
extremely hard in this task and in everything she did. … When Charlotte spoke, everybody
listened. She was never pedantic and always kept an open mind for the opinions of
others. … In her role as educator, Charlotte was responsible for teaching muscle physiology
to our
”Soon after I came to PCOM in 1989, I was asked to serve on a committee to revise
the faculty handbook and develop a tenure policy. Charlotte Greene was the chair of
the committee, which also included Michael Venditto, DO [now professor and chair,
Division of Pulmonary and Critical Care Medicine]. We had a big job to do. … Charlotte
was very knowledgeable about the multiple roles of faculty in an academic environment.
I enjoyed watching her pause for reflection, and if she didn’t have an immediate response,
she’d dig for information and come back to the table with advice for us. She worked
extremely hard in this task and in everything she did. … When Charlotte spoke, everybody
listened. She was never pedantic and always kept an open mind for the opinions of
others. … In her role as educator, Charlotte was responsible for teaching muscle physiology
to our 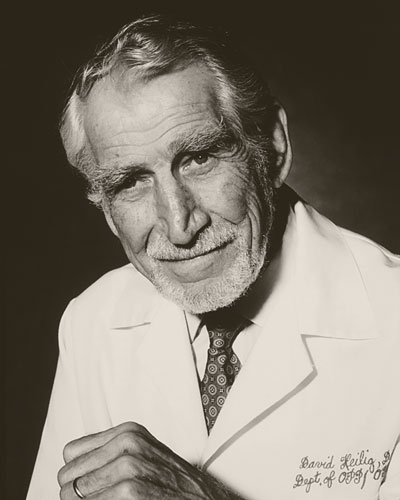 ”Dr. Heilig was my colleague and my mentor. But when I met him for the first time,
I was in seventh grade in my T-shirt and tighty-whities, waiting to get my physical
for football. Dr. Heilig told me to turn my head to the side and cough. … Basically,
because of my father [Nicholas S. Nicholas, DO, FAAO], I grew up with him. He was
a really important figure in our lives, kind of like a member of the family. But I
could never call him Dave; it was ‘Dr. Dave’ or ‘Doc Dave.’ … I didn’t see him much
while I was in medical school. But when my father was hired full-time to chair what’s
now the
”Dr. Heilig was my colleague and my mentor. But when I met him for the first time,
I was in seventh grade in my T-shirt and tighty-whities, waiting to get my physical
for football. Dr. Heilig told me to turn my head to the side and cough. … Basically,
because of my father [Nicholas S. Nicholas, DO, FAAO], I grew up with him. He was
a really important figure in our lives, kind of like a member of the family. But I
could never call him Dave; it was ‘Dr. Dave’ or ‘Doc Dave.’ … I didn’t see him much
while I was in medical school. But when my father was hired full-time to chair what’s
now the 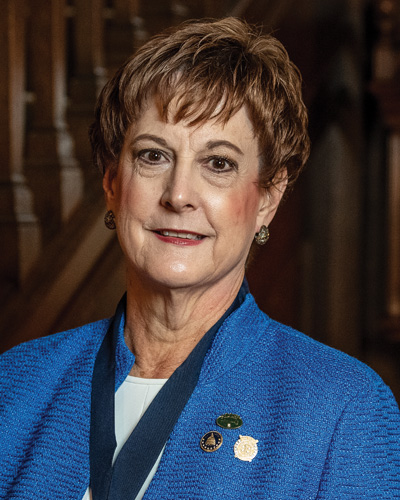 ”If we stand on the shoulders of giants, Carol is among the
”If we stand on the shoulders of giants, Carol is among the  “I met Joe about 10 years ago as a new physician working at Piedmont Urgent Care,
which was known as Wellstreet Urgent Care when we both started. … Dr. Joe, as we affectionately
call him, was a caring physician and a super-helpful colleague if I had a question
or was struggling with an electronic medical record in those first days. He had a
great bedside manner, and his patients seemed to love him. It was just a joy to work
alongside him. … I recently filled in at a center where he was working. I’m the regional
medical director now; Joe is a senior director. But it felt just like eight years
ago, when we last clinically worked side by side. He’s always jumping in, always making
sure that you know he’ll not only carry his load but help you if you need it. … Dr.
Joe is a wonderful clinician. He’s a listener, and he is intentional. So he finds
ways during a visit to connect with the patient, to make sure they know that during
that visit, they’re the only one who matters. He goes out of his way to provide that
customer service to a patient who needs it when they are usually at their worst and
facing someone they likely have never seen or spoken to before. He has some of the
highest patient satisfaction scores. … At the same time, he’s really fast! So I imagine
what happens is that he is in a hurry, but not in a rush. I think that his patients
forget about the length of the visit, because they recognize how meaningful it was.
… He’s also an excellent clinical teacher. Not everyone will or can latch on to his
efficiency; it’s something that has to be studied and learned. But his goal is for
that new physician or new advanced practice provider to take something that they can
tuck into their repertoire, and use it when they need to. … Dr. Joe gives back to
his school, to his profession, to his colleagues. He pours out to his patients that
which he has learned.”
“I met Joe about 10 years ago as a new physician working at Piedmont Urgent Care,
which was known as Wellstreet Urgent Care when we both started. … Dr. Joe, as we affectionately
call him, was a caring physician and a super-helpful colleague if I had a question
or was struggling with an electronic medical record in those first days. He had a
great bedside manner, and his patients seemed to love him. It was just a joy to work
alongside him. … I recently filled in at a center where he was working. I’m the regional
medical director now; Joe is a senior director. But it felt just like eight years
ago, when we last clinically worked side by side. He’s always jumping in, always making
sure that you know he’ll not only carry his load but help you if you need it. … Dr.
Joe is a wonderful clinician. He’s a listener, and he is intentional. So he finds
ways during a visit to connect with the patient, to make sure they know that during
that visit, they’re the only one who matters. He goes out of his way to provide that
customer service to a patient who needs it when they are usually at their worst and
facing someone they likely have never seen or spoken to before. He has some of the
highest patient satisfaction scores. … At the same time, he’s really fast! So I imagine
what happens is that he is in a hurry, but not in a rush. I think that his patients
forget about the length of the visit, because they recognize how meaningful it was.
… He’s also an excellent clinical teacher. Not everyone will or can latch on to his
efficiency; it’s something that has to be studied and learned. But his goal is for
that new physician or new advanced practice provider to take something that they can
tuck into their repertoire, and use it when they need to. … Dr. Joe gives back to
his school, to his profession, to his colleagues. He pours out to his patients that
which he has learned.” ”We acquired 130 acres of land in Moultrie, Colquitt County, right in the center of
Southwest Georgia. We donated 30 acres, and kept the remaining 100, and the College
”We acquired 130 acres of land in Moultrie, Colquitt County, right in the center of
Southwest Georgia. We donated 30 acres, and kept the remaining 100, and the College
 ”Up until the mid-1990s, PCOM’s entering classes of African American students were
very small. In my class (1989), entering in August of 1985, there were five African
Americans, four women and myself. Dr. Johnson made it a point to get to know all of
us. He made it a point to be nurturing. … He invited us over to his family medicine
practice in West Philadelphia to show us what it was like in private practice in the
inner-city African American community, and about the need for giving back and taking
care of people that were less fortunate. He also wanted us to see what was required
to own and manage a private practice, because most of us did not come from families
where Mom, Dad, or any family members were physicians. So he wanted to show us how
a practice could be set up—the functionality of it, the logistics—and I think he did
an excellent job. … Dr. Johnson was very devoted to young people and to helping them
recognize the importance of postsecondary education. Whether it was to study medicine,
engineering, law, nursing, teaching—he just wanted young people to pursue college.
… He was an amazing man, very driven. He wasn’t concerned about the number of hours
he put into the day. He would make rounds well into the evening after he finished
a long day of office hours and community engagements. It wasn’t unusual for him to
go to the hospital to finish rounds at 9 or 10 o’clock at night. Once office hours
ended, it was all about how he could reach out to the community beyond medicine. …
He was engaging and created relationships where patients could feel very comfortable
about confiding in him. He was a great mentor in helping to teach us how to
”Up until the mid-1990s, PCOM’s entering classes of African American students were
very small. In my class (1989), entering in August of 1985, there were five African
Americans, four women and myself. Dr. Johnson made it a point to get to know all of
us. He made it a point to be nurturing. … He invited us over to his family medicine
practice in West Philadelphia to show us what it was like in private practice in the
inner-city African American community, and about the need for giving back and taking
care of people that were less fortunate. He also wanted us to see what was required
to own and manage a private practice, because most of us did not come from families
where Mom, Dad, or any family members were physicians. So he wanted to show us how
a practice could be set up—the functionality of it, the logistics—and I think he did
an excellent job. … Dr. Johnson was very devoted to young people and to helping them
recognize the importance of postsecondary education. Whether it was to study medicine,
engineering, law, nursing, teaching—he just wanted young people to pursue college.
… He was an amazing man, very driven. He wasn’t concerned about the number of hours
he put into the day. He would make rounds well into the evening after he finished
a long day of office hours and community engagements. It wasn’t unusual for him to
go to the hospital to finish rounds at 9 or 10 o’clock at night. Once office hours
ended, it was all about how he could reach out to the community beyond medicine. …
He was engaging and created relationships where patients could feel very comfortable
about confiding in him. He was a great mentor in helping to teach us how to  ”I had been in practice for a year when I attended a continuing medical education
conference on new techniques for ENT. I sat across from Dr. Bill King, who said, ‘I’ve
never seen you before.’ He ended up inviting me to do some hours in his practice in
Germantown. That’s how it started, and I was there for about two years, before my
own practice got too busy for me to continue. A lot of doctors practicing now got
their start in Bill King’s office, picking up a few hours … Bill practiced in what
had been a huge funeral home, with beautiful waiting rooms to make his patients feel
valued. It was a very successful business—he rented space to a pharmacy, an X-ray
unit, a big physical therapy unit, all of them managed by his staff. … Saturday hours
were 7:00 a.m. to 7:00 p.m., and sometimes we wouldn’t get out till 9:00 or 10:00
p.m. I think I saw 86 patients one day. … He was particularly fond of the many children
in his practice, remembering most of their names and making up special names for some
… Bill had been a biochemist at the NIH National Heart Institute. On lunch breaks—though
we were so busy we hardly had any—he would talk to me about the disease process and
how medications affected it. … Bill had a gorgeous home, like a museum, with stuffed
animals and all kinds of carved masks and objects that he collected from his travels
around the world. His swimming pool was like a Hollywood setup. But he got delight
in seeing others’ delight in what he had. Some medical students got married in his
house; organizations had their meetings there. . . . What was really his thing was
philanthropy. He gave so much to the community. … He was a Central High alum and the
largest contributor to a new media center there, funded by alumni donations, that
opened in 2005. It was named for him. … He derived pleasure from what he was able
to do for other people. One day he said to me, ‘Bullock, come here. I have something
for you.’ He showed me a refrigerator full of prime rib. I had never set my eyes on
a chunk that big; I had to use a saw to get it into my fridge. It was absolutely the
best. That’s the way he was.”
”I had been in practice for a year when I attended a continuing medical education
conference on new techniques for ENT. I sat across from Dr. Bill King, who said, ‘I’ve
never seen you before.’ He ended up inviting me to do some hours in his practice in
Germantown. That’s how it started, and I was there for about two years, before my
own practice got too busy for me to continue. A lot of doctors practicing now got
their start in Bill King’s office, picking up a few hours … Bill practiced in what
had been a huge funeral home, with beautiful waiting rooms to make his patients feel
valued. It was a very successful business—he rented space to a pharmacy, an X-ray
unit, a big physical therapy unit, all of them managed by his staff. … Saturday hours
were 7:00 a.m. to 7:00 p.m., and sometimes we wouldn’t get out till 9:00 or 10:00
p.m. I think I saw 86 patients one day. … He was particularly fond of the many children
in his practice, remembering most of their names and making up special names for some
… Bill had been a biochemist at the NIH National Heart Institute. On lunch breaks—though
we were so busy we hardly had any—he would talk to me about the disease process and
how medications affected it. … Bill had a gorgeous home, like a museum, with stuffed
animals and all kinds of carved masks and objects that he collected from his travels
around the world. His swimming pool was like a Hollywood setup. But he got delight
in seeing others’ delight in what he had. Some medical students got married in his
house; organizations had their meetings there. . . . What was really his thing was
philanthropy. He gave so much to the community. … He was a Central High alum and the
largest contributor to a new media center there, funded by alumni donations, that
opened in 2005. It was named for him. … He derived pleasure from what he was able
to do for other people. One day he said to me, ‘Bullock, come here. I have something
for you.’ He showed me a refrigerator full of prime rib. I had never set my eyes on
a chunk that big; I had to use a saw to get it into my fridge. It was absolutely the
best. That’s the way he was.” “Dr. Kingsley didn’t start out in medicine as a researcher. But Jeff is every bit
the primary care physician he was when he came out of his residency in family medicine.
This is one of the most impressive features of who he is as a professional and as
a person. He and his clinical trial research company, Centricity, provide the highest
level of care to anyone that comes in the door. … He’s also committed to education
and mentoring. He opens his clinical trial centers for both medical students and residents
for rotations. And he feels—and I completely agree with him—that this is an essential
part of training. Healthcare providers have to appreciate and understand the clinical
trial process that
“Dr. Kingsley didn’t start out in medicine as a researcher. But Jeff is every bit
the primary care physician he was when he came out of his residency in family medicine.
This is one of the most impressive features of who he is as a professional and as
a person. He and his clinical trial research company, Centricity, provide the highest
level of care to anyone that comes in the door. … He’s also committed to education
and mentoring. He opens his clinical trial centers for both medical students and residents
for rotations. And he feels—and I completely agree with him—that this is an essential
part of training. Healthcare providers have to appreciate and understand the clinical
trial process that  ”Dr. Kvist was part of the reason I agreed to transition from pharmaceutical research
back into academia. I had been out of the teaching environment for probably a decade,
so I was nervous. He was a great mentor, able to advise without critiquing my personal
style. … Understanding how to present a dissected specimen to students on an exam
might seem straightforward, but there’s an art to it. And Dr. Kvist was able to guide
me and others to make sure we were assessing students in a fair but appropriate manner.
When I started here at PCOM, he had us sit down as a department and go through every
question on a written exam to make sure the scientific content was accurate. That
was his level of commitment to the reputation of the courses. … He was the first chair
of the
”Dr. Kvist was part of the reason I agreed to transition from pharmaceutical research
back into academia. I had been out of the teaching environment for probably a decade,
so I was nervous. He was a great mentor, able to advise without critiquing my personal
style. … Understanding how to present a dissected specimen to students on an exam
might seem straightforward, but there’s an art to it. And Dr. Kvist was able to guide
me and others to make sure we were assessing students in a fair but appropriate manner.
When I started here at PCOM, he had us sit down as a department and go through every
question on a written exam to make sure the scientific content was accurate. That
was his level of commitment to the reputation of the courses. … He was the first chair
of the 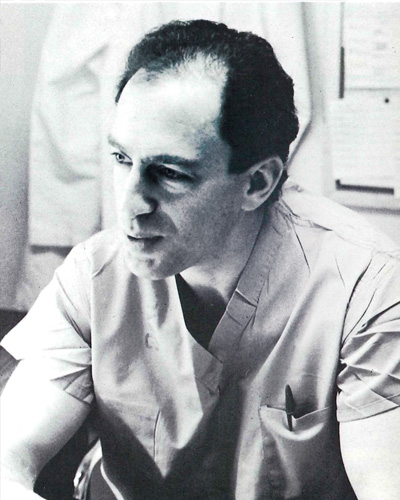 ”I graduated from medical school in 1995, did a year of internship in 1996, and spent
four years as a Navy flight surgeon and working with NASA. Then I took a year off
for my own transition as a transgender woman. … I had always hoped and dreamed to
be a plastic surgeon, and I went to Abington Hospital to jump back into my career.
My reviews were stellar, but they let me go. I was devastated and ended up switching
to Suburban Mercy Suburban Hospital for the four remaining years of general surgery.
Dr. Leis operated there too, and none of the other residents were interested in plastic
surgery, so there was nobody to help him. About a half-dozen plastic surgeons rotated
through that hospital, so I ended up getting this incredible plastic surgery experience.
I was in the right place at the right time. … Dr. Leis created the Plastic and Reconstructive
Surgery residency at PCOM in 1991, and he’s really the father of plastic surgery for
the osteopathic profession. None of us would be here if it weren’t for him. When I
was trying to get into a plastic surgery residency, there were only three spots in
the whole country that a DO could qualify for. I was one of two people selected for
the PCOM program that year. … At that time, hospitals in Philadelphia were closing,
selling, restructuring—it was like musical chairs. Dr. Leis fought hard to get into
places where previously only MDs got in. He wanted to make sure we had a full and
balanced education. We were in five or six different hospitals, and it’s made all
the difference in the breadth of my skills. … In the middle of my rotation with him,
he became ill and was out of commission for a couple of months. I had to go make my
own residency, which enabled me to get some very specialized training in transgender
medicine. … Dr. Leis listened to people, and everyone came in as an equal. No matter
how down and out somebody was when they came to see him, he would listen to them and
try to help them. … He was an innovator, and he didn’t limit himself. At conferences,
he always asked about controversial subjects. He challenged people, and he stood up
for what he believed in.”
”I graduated from medical school in 1995, did a year of internship in 1996, and spent
four years as a Navy flight surgeon and working with NASA. Then I took a year off
for my own transition as a transgender woman. … I had always hoped and dreamed to
be a plastic surgeon, and I went to Abington Hospital to jump back into my career.
My reviews were stellar, but they let me go. I was devastated and ended up switching
to Suburban Mercy Suburban Hospital for the four remaining years of general surgery.
Dr. Leis operated there too, and none of the other residents were interested in plastic
surgery, so there was nobody to help him. About a half-dozen plastic surgeons rotated
through that hospital, so I ended up getting this incredible plastic surgery experience.
I was in the right place at the right time. … Dr. Leis created the Plastic and Reconstructive
Surgery residency at PCOM in 1991, and he’s really the father of plastic surgery for
the osteopathic profession. None of us would be here if it weren’t for him. When I
was trying to get into a plastic surgery residency, there were only three spots in
the whole country that a DO could qualify for. I was one of two people selected for
the PCOM program that year. … At that time, hospitals in Philadelphia were closing,
selling, restructuring—it was like musical chairs. Dr. Leis fought hard to get into
places where previously only MDs got in. He wanted to make sure we had a full and
balanced education. We were in five or six different hospitals, and it’s made all
the difference in the breadth of my skills. … In the middle of my rotation with him,
he became ill and was out of commission for a couple of months. I had to go make my
own residency, which enabled me to get some very specialized training in transgender
medicine. … Dr. Leis listened to people, and everyone came in as an equal. No matter
how down and out somebody was when they came to see him, he would listen to them and
try to help them. … He was an innovator, and he didn’t limit himself. At conferences,
he always asked about controversial subjects. He challenged people, and he stood up
for what he believed in.” “Jim’s a very interesting man, a real visionary. Sometimes people will say, when they
hear one of his ideas, ‘Why Moultrie?’ He just says, ‘Why not Moultrie? What’s stopping
us? Nothing’s stopping us if we want to do something.’ That’s how he lives his life.
… Jim started a family medicine residency to not only help with recruiting physicians
to his facility but because he knew that a training program would increase and enhance
the quality of care at the hospital. … After that, Jim felt strongly that the area
needed a medical school. He said, ‘You know, if we give the regional students a place
to go to medical school and train them here, we can keep them here.’ . . . I’ve watched
how he has grown the hospital at
“Jim’s a very interesting man, a real visionary. Sometimes people will say, when they
hear one of his ideas, ‘Why Moultrie?’ He just says, ‘Why not Moultrie? What’s stopping
us? Nothing’s stopping us if we want to do something.’ That’s how he lives his life.
… Jim started a family medicine residency to not only help with recruiting physicians
to his facility but because he knew that a training program would increase and enhance
the quality of care at the hospital. … After that, Jim felt strongly that the area
needed a medical school. He said, ‘You know, if we give the regional students a place
to go to medical school and train them here, we can keep them here.’ . . . I’ve watched
how he has grown the hospital at  ”Bob was my teacher and my colleague. As a teacher, he was brilliant. Yet, I don’t
think he ever recognized his own genius—how he informed his art with fresh perspective,
sage advice and a hint of silliness. … On the first day of class, we were thrown into
a big auditorium. During the course of his radiology presentation, Bob would put up
someone’s picture on that big screen and ask us to answer his clinical question. We
usually had no idea what he was talking about. Perhaps that was our first reality
check: ‘Boy, we’re really in medical school now.’ But very quickly, we realized that
he was not concerned about our answers. He was more focused on creating an encouraging
educational environment, in every class, to take away some of our paranoia about making
a mistake. The wisdom of his teaching was understanding that only when you let go
do you open yourself up to learn. … Years later, I was fortunate to have an office
very close to where he taught the third-year students. There was a mandatory radiology
clerkship; you had to experience Bob regardless of whether you wanted to be a radiologist
or a family doctor or an internist. During the first week, it was kind of quiet in
that classroom. By the beginning of the second week, you’d hear laughter, singing,
all kinds of shenanigans. He had puppets; he was Mister Rogers before Mister Rogers.
He would have the students whistling, humming, playing guitars, doing skits. … What
could be more embarrassing than standing in front of your peers and singing? But once
you got over that embarrassment, you opened yourself up to learning. … Bob hasn’t
been with us for a number of years; he passed away in 2005. But hospital administrators—across
the state and region—still tell me they can identify PCOM grads because they’re not
intimidated by reading images and films. They never have that deer-in-a-headlight
look. They know logically how to look through the film, look at the soft tissue, the
anatomical components. … Bob won teaching awards over and over again. … He told me,
‘This is how I enjoy teaching.’ The excitement, the enthusiasm, the energy that he
created in his classroom came back to him, made him more spirited and more inclined
to give. … Even when he got sick at the end, he never retired. His enjoyment of teaching
actually penetrated the classroom. You can pick that up as a student. If the teacher
is excited about being in front of you, that goes a long way.”
”Bob was my teacher and my colleague. As a teacher, he was brilliant. Yet, I don’t
think he ever recognized his own genius—how he informed his art with fresh perspective,
sage advice and a hint of silliness. … On the first day of class, we were thrown into
a big auditorium. During the course of his radiology presentation, Bob would put up
someone’s picture on that big screen and ask us to answer his clinical question. We
usually had no idea what he was talking about. Perhaps that was our first reality
check: ‘Boy, we’re really in medical school now.’ But very quickly, we realized that
he was not concerned about our answers. He was more focused on creating an encouraging
educational environment, in every class, to take away some of our paranoia about making
a mistake. The wisdom of his teaching was understanding that only when you let go
do you open yourself up to learn. … Years later, I was fortunate to have an office
very close to where he taught the third-year students. There was a mandatory radiology
clerkship; you had to experience Bob regardless of whether you wanted to be a radiologist
or a family doctor or an internist. During the first week, it was kind of quiet in
that classroom. By the beginning of the second week, you’d hear laughter, singing,
all kinds of shenanigans. He had puppets; he was Mister Rogers before Mister Rogers.
He would have the students whistling, humming, playing guitars, doing skits. … What
could be more embarrassing than standing in front of your peers and singing? But once
you got over that embarrassment, you opened yourself up to learning. … Bob hasn’t
been with us for a number of years; he passed away in 2005. But hospital administrators—across
the state and region—still tell me they can identify PCOM grads because they’re not
intimidated by reading images and films. They never have that deer-in-a-headlight
look. They know logically how to look through the film, look at the soft tissue, the
anatomical components. … Bob won teaching awards over and over again. … He told me,
‘This is how I enjoy teaching.’ The excitement, the enthusiasm, the energy that he
created in his classroom came back to him, made him more spirited and more inclined
to give. … Even when he got sick at the end, he never retired. His enjoyment of teaching
actually penetrated the classroom. You can pick that up as a student. If the teacher
is excited about being in front of you, that goes a long way.” ”When I first joined the College as a young professor, I shadowed Roe. As my faculty
mentor, she’d often meet and walk me from classes and around campus. It always amazed
me that we’d never make it more than a few yards (sometimes a few footsteps) without
students, faculty and staff stopping us. Everyone wanted to talk to Roe—professionally.
Personally. I think they simply wanted to experience the warmth of her presence, her
benevolence. Her authenticity. She puts everyone at ease. … In psychology, we teach
that empathy starts with being present. Roe is always fully present as a person, as
a teacher, as a therapist, as a leader. She is a nurturer. At the same time, she is
strong, assertive and effective. … She brought a whole lifetime with her when she
came to PCOM. She had been a fourth-grade teacher, a guidance counselor, a school
psychologist in the New Jersey public schools. She is also a doting mother to her
daughter. She recognized that she had grown and matured throughout her career and
the many different facets of it. She worked at PCOM for nearly a decade (before her
retirement in 2014) and during that time developed, implemented and taught three
”When I first joined the College as a young professor, I shadowed Roe. As my faculty
mentor, she’d often meet and walk me from classes and around campus. It always amazed
me that we’d never make it more than a few yards (sometimes a few footsteps) without
students, faculty and staff stopping us. Everyone wanted to talk to Roe—professionally.
Personally. I think they simply wanted to experience the warmth of her presence, her
benevolence. Her authenticity. She puts everyone at ease. … In psychology, we teach
that empathy starts with being present. Roe is always fully present as a person, as
a teacher, as a therapist, as a leader. She is a nurturer. At the same time, she is
strong, assertive and effective. … She brought a whole lifetime with her when she
came to PCOM. She had been a fourth-grade teacher, a guidance counselor, a school
psychologist in the New Jersey public schools. She is also a doting mother to her
daughter. She recognized that she had grown and matured throughout her career and
the many different facets of it. She worked at PCOM for nearly a decade (before her
retirement in 2014) and during that time developed, implemented and taught three  ”My dad was a larger-than-life figure. He came to Philadelphia in 1946 after his discharge
from the United States Navy. A first-generation Greek immigrant, he discovered Philadelphia
College of Osteopathy on 48th and Spruce streets, where he took continuing medical
education classes and soon started teaching
”My dad was a larger-than-life figure. He came to Philadelphia in 1946 after his discharge
from the United States Navy. A first-generation Greek immigrant, he discovered Philadelphia
College of Osteopathy on 48th and Spruce streets, where he took continuing medical
education classes and soon started teaching  ”Our favorite hangout was the study room. That’s where you’d often find Jason, James
[Lindsay, PharmD ’14] and me, cracking jokes while perusing our pharmacology books.
More than a few times, Jason retreated there on his own to lie on the floor and to
pray the pain of sickle cell anemia away—once in the middle of an exam. … Our study
room now bears Jason’s name, dedicated in loving memory to my best friend and fellow
graduate of PCOM’s inaugural PharmD class, a lasting tribute to Jason Walton O’Neal’s
grit, gumption and sly smile I’d do anything to see again. … Complications from sickle
cell disease took Jason from us on August 12, 2016, too young at age 35 and only two
years after he’d accomplished his goal of
”Our favorite hangout was the study room. That’s where you’d often find Jason, James
[Lindsay, PharmD ’14] and me, cracking jokes while perusing our pharmacology books.
More than a few times, Jason retreated there on his own to lie on the floor and to
pray the pain of sickle cell anemia away—once in the middle of an exam. … Our study
room now bears Jason’s name, dedicated in loving memory to my best friend and fellow
graduate of PCOM’s inaugural PharmD class, a lasting tribute to Jason Walton O’Neal’s
grit, gumption and sly smile I’d do anything to see again. … Complications from sickle
cell disease took Jason from us on August 12, 2016, too young at age 35 and only two
years after he’d accomplished his goal of  ”In July 2005, I came with Mary and several others to develop the curriculum that
would start in mid-August at the new Georgia campus of PCOM. It was quite a task to
get all those ducks in a row, tweaking the Philadelphia curriculum and figuring out
who was doing what. For several weeks before our offices were ready, we worked in
an old house at the Osteopathic Institute of the South. It drove home the fact that
we were starting from the ground up. … We were from all over the place—except Mary,
our only southerner, who was from Alabama. … Her work and experience in pharmacology
helped her put together the initial curriculum. She had so many accomplishments, but
she was very humble about them. She was also a very private person, and very independent.
… Mary became an influential person on the
”In July 2005, I came with Mary and several others to develop the curriculum that
would start in mid-August at the new Georgia campus of PCOM. It was quite a task to
get all those ducks in a row, tweaking the Philadelphia curriculum and figuring out
who was doing what. For several weeks before our offices were ready, we worked in
an old house at the Osteopathic Institute of the South. It drove home the fact that
we were starting from the ground up. … We were from all over the place—except Mary,
our only southerner, who was from Alabama. … Her work and experience in pharmacology
helped her put together the initial curriculum. She had so many accomplishments, but
she was very humble about them. She was also a very private person, and very independent.
… Mary became an influential person on the  “There are a handful of students that you just bond with from the very beginning,
and Greg was one of them. I was director of admissions when he applied to PCOM, so
I would have been the initial reviewer of his application. Coming from San Diego State,
Greg considered PCOM his first choice of schools because of our reputation. … I got
to know Greg well. He was an outstanding student from day one. And he was always participating
in what was going on, always volunteering. He took part in a video we made for student
recruitment, and I remember him saying that medical school is like hooking yourself
up to a fire hydrant and turning it on. … We often see Greg at professional annual
meetings. And although he’s a Denver native and lives in a Denver suburb now, he visits
our campus when he can, and often brings his family with him. He has not lost contact
with PCOM since the day he graduated. … For almost 10 years, he’s been contributing
to the Dr. and Mrs. Gregory G. Papadeas & Family Endowed Scholarship, which provides
tuition support to DO students of Greek heritage. He loved PCOM from the beginning,
and he feels it did well by him and that his PCOM education propelled him into being
an outstanding physician. He’s proud of the school, and he’s proud of being a DO.
… In 2019, he hosted a cocktail party at his home for local PCOM alumni and other
DOs. I was thrilled to be invited also. It was a wonderful weekend, the party was
magnificent, and we all enjoyed the time spent with his lovely family. Greg is fun
to be with, sincere and warm. He is one of the finest PCOM graduates that I know.”
“There are a handful of students that you just bond with from the very beginning,
and Greg was one of them. I was director of admissions when he applied to PCOM, so
I would have been the initial reviewer of his application. Coming from San Diego State,
Greg considered PCOM his first choice of schools because of our reputation. … I got
to know Greg well. He was an outstanding student from day one. And he was always participating
in what was going on, always volunteering. He took part in a video we made for student
recruitment, and I remember him saying that medical school is like hooking yourself
up to a fire hydrant and turning it on. … We often see Greg at professional annual
meetings. And although he’s a Denver native and lives in a Denver suburb now, he visits
our campus when he can, and often brings his family with him. He has not lost contact
with PCOM since the day he graduated. … For almost 10 years, he’s been contributing
to the Dr. and Mrs. Gregory G. Papadeas & Family Endowed Scholarship, which provides
tuition support to DO students of Greek heritage. He loved PCOM from the beginning,
and he feels it did well by him and that his PCOM education propelled him into being
an outstanding physician. He’s proud of the school, and he’s proud of being a DO.
… In 2019, he hosted a cocktail party at his home for local PCOM alumni and other
DOs. I was thrilled to be invited also. It was a wonderful weekend, the party was
magnificent, and we all enjoyed the time spent with his lovely family. Greg is fun
to be with, sincere and warm. He is one of the finest PCOM graduates that I know.” ”Rich was the director of medical education when I was a resident, so I got to know
him at morning reports and at lectures. The big thing with Rich is his personality—he’s
easy to talk to, very engaging, and makes you feel like you’re the most important
person in the room. And he always used humor to break the ice or put people at ease
in a meeting. … He asked me in 2005 to become the associate program director for the
Family Medicine residency, and in that position I reported to him. In 2012, when he
was the vice dean for
”Rich was the director of medical education when I was a resident, so I got to know
him at morning reports and at lectures. The big thing with Rich is his personality—he’s
easy to talk to, very engaging, and makes you feel like you’re the most important
person in the room. And he always used humor to break the ice or put people at ease
in a meeting. … He asked me in 2005 to become the associate program director for the
Family Medicine residency, and in that position I reported to him. In 2012, when he
was the vice dean for  ”Julia arrived as one of our inaugural students from a small nearby town, Tifton.
I was assigned to check in with her regularly as her faculty mentor … The first six
or eight weeks of the
”Julia arrived as one of our inaugural students from a small nearby town, Tifton.
I was assigned to check in with her regularly as her faculty mentor … The first six
or eight weeks of the  ”Nick Pedano was my guide and counselor—and also my cousin. My grandmother was a Pedano.
… When I decided I wanted to go to PCOM, Nick wrote a letter for me. Later, when I
had a little trouble with anatomy, Nick talked to his close friend Angus Cathie [then
chair of the department]. …Nick wanted me to be a surgeon, even though I said, ‘Nick,
I’m not good with my hands.’ … I remember one case, the second operation was 12 hours.
I’m short, so I had to stand on a stool, and I said, ‘Maybe it’s better if I pass
out.’ After it was over and we were taking the gloves off, I said, ‘Cuz, this is not
for me.’ He said, ‘All right. You’re going to go into internal medicine.’ … Nick could
order you to do something and you did it, and then— ‘Wait a minute, what am I doing?’
… The whole family had a commanding presence. Surgeons have to be commanding, and
they have to give orders, but they get away with more if the iron fist has a velvet
glove. … There were two parts of Nick’s personality. He was friendly, and he was bossy—but
he had a nice way about him. … He had a house down the shore in Margate, right by
the ocean, and he would have a party every year for the interns and for the residents,
a beautiful affair. He would wine and dine them because he appreciated what they did
for him. And he developed relationships all the way up the line. That was the social
Nick. In the operating room, he took no hostages, because he had to get things done
the way he wanted them done. … As chairman of surgery, Nick led the way to the growth
of PCOM by example. He had a massive service, with tons of patients. He went all over
the place to nurture family doctors. … The people who worked with him were indefatigable
and inextinguishable. The College is to a large degree where it is because of his
absolutely brilliant energy. … From Nick, I saw that leadership is not totally dictatorial
or totally social. It’s a good mixture of both. So I try to achieve that balance with
my house staff. Yes, we work hard. When it comes time for me to be the boss, they
look at me as the boss. But then I’ll say, ‘Okay, it’s five o’clock, let’s go over
to the Hilton.’ ”
”Nick Pedano was my guide and counselor—and also my cousin. My grandmother was a Pedano.
… When I decided I wanted to go to PCOM, Nick wrote a letter for me. Later, when I
had a little trouble with anatomy, Nick talked to his close friend Angus Cathie [then
chair of the department]. …Nick wanted me to be a surgeon, even though I said, ‘Nick,
I’m not good with my hands.’ … I remember one case, the second operation was 12 hours.
I’m short, so I had to stand on a stool, and I said, ‘Maybe it’s better if I pass
out.’ After it was over and we were taking the gloves off, I said, ‘Cuz, this is not
for me.’ He said, ‘All right. You’re going to go into internal medicine.’ … Nick could
order you to do something and you did it, and then— ‘Wait a minute, what am I doing?’
… The whole family had a commanding presence. Surgeons have to be commanding, and
they have to give orders, but they get away with more if the iron fist has a velvet
glove. … There were two parts of Nick’s personality. He was friendly, and he was bossy—but
he had a nice way about him. … He had a house down the shore in Margate, right by
the ocean, and he would have a party every year for the interns and for the residents,
a beautiful affair. He would wine and dine them because he appreciated what they did
for him. And he developed relationships all the way up the line. That was the social
Nick. In the operating room, he took no hostages, because he had to get things done
the way he wanted them done. … As chairman of surgery, Nick led the way to the growth
of PCOM by example. He had a massive service, with tons of patients. He went all over
the place to nurture family doctors. … The people who worked with him were indefatigable
and inextinguishable. The College is to a large degree where it is because of his
absolutely brilliant energy. … From Nick, I saw that leadership is not totally dictatorial
or totally social. It’s a good mixture of both. So I try to achieve that balance with
my house staff. Yes, we work hard. When it comes time for me to be the boss, they
look at me as the boss. But then I’ll say, ‘Okay, it’s five o’clock, let’s go over
to the Hilton.’ ” ”When I began
”When I began  ”When I started teaching at PCOM, I listened to tapes that students had made of JoAnne’s
lectures. It was so easy to follow her. JoAnne was a very good teacher. … She always
had a smile. I remember giving one lecture when I had just started teaching. Those
lecture rooms are huge, holding about 270 people. And there she was in the audience,
near the front. At one point when I looked up, she had the best smile on her face.
It was such a wonderful thing to see. … JoAnne was probably about five foot four or
five, with short, straight hair and looked like she would be no-nonsense. And in some
cases she was; she was a strong woman. But really, she was just fun. She never got
frustrated with me, with students, with anybody. Students loved her! … When JoAnne
met Barbara [now Dr. Thornton’s spouse] and me, we were a couple. We remember going
to events and how welcoming she was of both of us. She was always interested in people.
… JoAnne’s field was lipids—so was her husband’s [Ronald Pieringer, PhD, was Dr. Thornton’s
professor when she was a doctoral student at Temple University]—and that’s not my
favorite subject. So she and I complemented each other intellectually. … JoAnne had
her own research. But when Dr. Mochan [Eugene Mochan, PhD, DO ’77, then department
chair] was there, he had a particular research project in molecular biology he wanted
the department to do. JoAnne was able to shift gears on this ongoing project. She
was a kind of gung-ho type of person: ‘I’m just going to jump in here, and I’m going
to do it. And I’m going to enjoy it.’… I became the chair of the department after
Dr. Mochan stepped down. I found that a lot of my ideas about how to approach students
and how to manage people had come from JoAnne. We only overlapped for perhaps two
years before she passed away, and I didn’t realize at the time how much I was getting
from her. There was no expectation of her being my mentor; it just happened. …When
she died, Dr. Mochan, Dr. Ruth Borghaei and I set up a scholarship fund in JoAnne’s
name, along with a brick laid in the Donor Garden outside Evans Hall.”
”When I started teaching at PCOM, I listened to tapes that students had made of JoAnne’s
lectures. It was so easy to follow her. JoAnne was a very good teacher. … She always
had a smile. I remember giving one lecture when I had just started teaching. Those
lecture rooms are huge, holding about 270 people. And there she was in the audience,
near the front. At one point when I looked up, she had the best smile on her face.
It was such a wonderful thing to see. … JoAnne was probably about five foot four or
five, with short, straight hair and looked like she would be no-nonsense. And in some
cases she was; she was a strong woman. But really, she was just fun. She never got
frustrated with me, with students, with anybody. Students loved her! … When JoAnne
met Barbara [now Dr. Thornton’s spouse] and me, we were a couple. We remember going
to events and how welcoming she was of both of us. She was always interested in people.
… JoAnne’s field was lipids—so was her husband’s [Ronald Pieringer, PhD, was Dr. Thornton’s
professor when she was a doctoral student at Temple University]—and that’s not my
favorite subject. So she and I complemented each other intellectually. … JoAnne had
her own research. But when Dr. Mochan [Eugene Mochan, PhD, DO ’77, then department
chair] was there, he had a particular research project in molecular biology he wanted
the department to do. JoAnne was able to shift gears on this ongoing project. She
was a kind of gung-ho type of person: ‘I’m just going to jump in here, and I’m going
to do it. And I’m going to enjoy it.’… I became the chair of the department after
Dr. Mochan stepped down. I found that a lot of my ideas about how to approach students
and how to manage people had come from JoAnne. We only overlapped for perhaps two
years before she passed away, and I didn’t realize at the time how much I was getting
from her. There was no expectation of her being my mentor; it just happened. …When
she died, Dr. Mochan, Dr. Ruth Borghaei and I set up a scholarship fund in JoAnne’s
name, along with a brick laid in the Donor Garden outside Evans Hall.” “There were 17 students in Dave’s cohort who attended all the classes in the program
together and then went on to complete their internships and dissertations. They were
a very tight group, and I think Dave was one of the biggest reasons for that. He has
a terrific sense of humor; he’s very positive and open, and the other students warmed
up to him quickly. Dave asked excellent questions in class, but he would also make
some very funny comments. … I got to know Dave much better when I served on his dissertation
committee. And again, he always had an open mind, a positive attitude, and a willingness
to dig in and do what needed to be done. … After Dave received his degree, he was
recruited as one of the adjuncts to teach for us. He was also invited to serve on
the
“There were 17 students in Dave’s cohort who attended all the classes in the program
together and then went on to complete their internships and dissertations. They were
a very tight group, and I think Dave was one of the biggest reasons for that. He has
a terrific sense of humor; he’s very positive and open, and the other students warmed
up to him quickly. Dave asked excellent questions in class, but he would also make
some very funny comments. … I got to know Dave much better when I served on his dissertation
committee. And again, he always had an open mind, a positive attitude, and a willingness
to dig in and do what needed to be done. … After Dave received his degree, he was
recruited as one of the adjuncts to teach for us. He was also invited to serve on
the  ”When I was a little girl in Columbus, Ohio, my father was head of the Radiology Department
at Doctors Hospital. I rode with him to the hospital, and the school bus picked me
up at the emergency entrance. So I stood there in the hall looking at the window,
waiting for the school bus. Dr. Purdy would come by and say hello to me. She was the
first woman physician I knew [and the first at Doctors Hospital—a woman who would
successfully lobby for the first ICU unit in the state.] … She and my father got along
very well. Once, Dr. Purdy’s Mercedes was making some sort of a noise, and my father
said he’d trade cars with her for two days and figure out what it was. But the next
day she gave his back. She’d been driving on US Highway 33. My father was the chief
of the volunteer fire department, and she had somehow flipped the switch in his car
that turned the horn into a siren and lights. … I had been a geologist, and when I
decided to go to medical school I could really count on my fingers the number of people
who thought that was a good idea. But fortunately my husband [George O. Faerber, DO
’61] was on that list, and Dr. Purdy was too. … When I graduated from medical school,
she sent me a card that said, ‘Congratulations on your degree. Now that you’re done
with your academic work, you’ll have to work harder, be smarter. … ’ Inside it said,
‘But being a woman like you, that won’t be hard.’ … I did my training after medical
school at Doctors Hospital. She and another woman internist said essentially the same
thing to me: I could run something past them with no worry that they were going to
say, ‘What do you mean?’ . … Dr. Purdy was a reserved person, but she was friendly
and warm. She cared for her patients, and she cared for her friends. … Later on, Dr.
Purdy and I shared offices. I was in her office, right at the hospital, one morning
a week, with her staff, and one morning a week she was in my office, in an urban area
with marvelous parking, with my staff. We didn’t have any financial arrangement. We
had a woman’s handshake on it. That arrangement lasted over a decade, until I sold
my practice.”
”When I was a little girl in Columbus, Ohio, my father was head of the Radiology Department
at Doctors Hospital. I rode with him to the hospital, and the school bus picked me
up at the emergency entrance. So I stood there in the hall looking at the window,
waiting for the school bus. Dr. Purdy would come by and say hello to me. She was the
first woman physician I knew [and the first at Doctors Hospital—a woman who would
successfully lobby for the first ICU unit in the state.] … She and my father got along
very well. Once, Dr. Purdy’s Mercedes was making some sort of a noise, and my father
said he’d trade cars with her for two days and figure out what it was. But the next
day she gave his back. She’d been driving on US Highway 33. My father was the chief
of the volunteer fire department, and she had somehow flipped the switch in his car
that turned the horn into a siren and lights. … I had been a geologist, and when I
decided to go to medical school I could really count on my fingers the number of people
who thought that was a good idea. But fortunately my husband [George O. Faerber, DO
’61] was on that list, and Dr. Purdy was too. … When I graduated from medical school,
she sent me a card that said, ‘Congratulations on your degree. Now that you’re done
with your academic work, you’ll have to work harder, be smarter. … ’ Inside it said,
‘But being a woman like you, that won’t be hard.’ … I did my training after medical
school at Doctors Hospital. She and another woman internist said essentially the same
thing to me: I could run something past them with no worry that they were going to
say, ‘What do you mean?’ . … Dr. Purdy was a reserved person, but she was friendly
and warm. She cared for her patients, and she cared for her friends. … Later on, Dr.
Purdy and I shared offices. I was in her office, right at the hospital, one morning
a week, with her staff, and one morning a week she was in my office, in an urban area
with marvelous parking, with my staff. We didn’t have any financial arrangement. We
had a woman’s handshake on it. That arrangement lasted over a decade, until I sold
my practice.” “Art Freeman, my late predecessor and mentor, who brought me to PCOM, had a vision
for psychology that included not only high-quality education and training but giving
back by offering continuing education to practitioners in the community. The department
had a program that had been called the Friday Night Speaker Series. But when it became
the
“Art Freeman, my late predecessor and mentor, who brought me to PCOM, had a vision
for psychology that included not only high-quality education and training but giving
back by offering continuing education to practitioners in the community. The department
had a program that had been called the Friday Night Speaker Series. But when it became
the  “When the
“When the  ”I worked with Ida Schmidt one day a week for almost the last 10 years of her life.
I had a wonderful experience with her. When I started in the
”I worked with Ida Schmidt one day a week for almost the last 10 years of her life.
I had a wonderful experience with her. When I started in the  ”John and I were together for a very long time. I first met John as a medical student
through his academic courses and lectures and on his pulmonary service. He also taught
me during my internship at Metropolitan Hospital. I went into practice with him in
1995, and we worked together until his retirement in 2018. … John was an exceptional
clinician and a tireless advocate for compassionate patient care. He was also a jokester.
He liked to laugh. He had an uncanny ability to connect with people—all people at all times. His patients loved him; they would travel great distances to be seen by him.
… He was a beloved teacher. Throughout his career he taught thousands of students,
interns and residents. They genuinely adored him—and he endearingly referred to them
as his “kids.” Year after year, he’d be
”John and I were together for a very long time. I first met John as a medical student
through his academic courses and lectures and on his pulmonary service. He also taught
me during my internship at Metropolitan Hospital. I went into practice with him in
1995, and we worked together until his retirement in 2018. … John was an exceptional
clinician and a tireless advocate for compassionate patient care. He was also a jokester.
He liked to laugh. He had an uncanny ability to connect with people—all people at all times. His patients loved him; they would travel great distances to be seen by him.
… He was a beloved teacher. Throughout his career he taught thousands of students,
interns and residents. They genuinely adored him—and he endearingly referred to them
as his “kids.” Year after year, he’d be  “Clyde likes to say that he and Sandra are an open book; what you see is what you
get. They are both originally from North Carolina. They love Gwinnett County, they
love family; they love God first. They’re what my great-grandmother would call the
salt of the earth—just good people. … Clyde pulled himself up by his own bootstraps.
At one point he collected mounds of dirt, and drove out of town to sell them for $5
a load. He realized he could sell four or five loads before he went to his job and
make more money than he did from that job, which paid $1.78 an hour. That story stuck
with me. When Clyde tells you these stories, you’ve just got to listen, because if
you don’t, you will miss something. … Sandra and Clyde are equally yoked. They have
two different skill sets, but I feel that they’re both primary in their relationship—strong
complements to one another. Sandra likes to call herself a city girl, because in the
area of North Carolina where they grew up, she was more in the city. She has the same
commitment to God and faith and family, the same commitment to hard work. I would
guess that they have not made a major decision one without the other. … Their name
is on everything in this community. We know about the gifts to the hospital, the football
field at a local high school, the main stage at a local theater, and their support
of community non-profits and education. … When they made their gift to PCOM, the
“Clyde likes to say that he and Sandra are an open book; what you see is what you
get. They are both originally from North Carolina. They love Gwinnett County, they
love family; they love God first. They’re what my great-grandmother would call the
salt of the earth—just good people. … Clyde pulled himself up by his own bootstraps.
At one point he collected mounds of dirt, and drove out of town to sell them for $5
a load. He realized he could sell four or five loads before he went to his job and
make more money than he did from that job, which paid $1.78 an hour. That story stuck
with me. When Clyde tells you these stories, you’ve just got to listen, because if
you don’t, you will miss something. … Sandra and Clyde are equally yoked. They have
two different skill sets, but I feel that they’re both primary in their relationship—strong
complements to one another. Sandra likes to call herself a city girl, because in the
area of North Carolina where they grew up, she was more in the city. She has the same
commitment to God and faith and family, the same commitment to hard work. I would
guess that they have not made a major decision one without the other. … Their name
is on everything in this community. We know about the gifts to the hospital, the football
field at a local high school, the main stage at a local theater, and their support
of community non-profits and education. … When they made their gift to PCOM, the 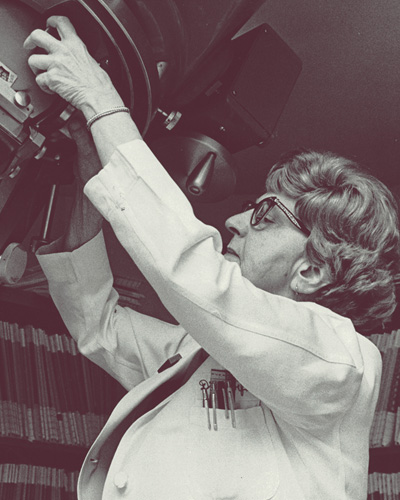 ”Dr. Swift was a long-term member of the Radiology Department at PCOM [retired as
vice chairman of the department]. I was a resident, and she was one of my mentors.
She was a very organized person and believed that if you conducted procedures in an
orderly fashion, you would be rewarded with good, accurate outcomes. … On one occasion,
I was attempting to do a barium enema—introduce barium into the patient’s colon. It
was a catastrophe. The barium was not in the patient’s colon. It was on the patient,
on me, on the table, on the floor, on the technician. I had failed in a dramatic and
humiliating way. I remember that exam to this day. . . . Dr. Swift looked into the
room and said, ‘Can I give you a hand?’” I said a grateful ‘Yes.’ She helped clean
up the mess, and we started again. She established a quietly competent atmosphere,
and we successfully completed the exam. I expected a sharp critique, but she said,
‘I know you know how to do this exam, and you had a bad day. There will be bad days.’
… I joined the department after I completed my residency training. She knew when to
be critical and when to be just human and supportive. She showed me how to treat the
people I was training. … Dr. Swift was a formal person 99 percent of the time. You
knew that there was more to her, but you didn’t get a look at it very often. … She
did the mammography at the hospital and didn’t have a lot of time for other things.
But I knew that I could go to her and say, ‘Look, I’m in a conundrum with this particular
case. I just don’t know which way to go.’ As a radiologist, you want to be careful
not to give people reasons to do a tremendous amount of additional studies that don’t
go anywhere. On the other hand, you don’t want to overlook anything. Dr. Swift was
really good at that. I could count on her.”
”Dr. Swift was a long-term member of the Radiology Department at PCOM [retired as
vice chairman of the department]. I was a resident, and she was one of my mentors.
She was a very organized person and believed that if you conducted procedures in an
orderly fashion, you would be rewarded with good, accurate outcomes. … On one occasion,
I was attempting to do a barium enema—introduce barium into the patient’s colon. It
was a catastrophe. The barium was not in the patient’s colon. It was on the patient,
on me, on the table, on the floor, on the technician. I had failed in a dramatic and
humiliating way. I remember that exam to this day. . . . Dr. Swift looked into the
room and said, ‘Can I give you a hand?’” I said a grateful ‘Yes.’ She helped clean
up the mess, and we started again. She established a quietly competent atmosphere,
and we successfully completed the exam. I expected a sharp critique, but she said,
‘I know you know how to do this exam, and you had a bad day. There will be bad days.’
… I joined the department after I completed my residency training. She knew when to
be critical and when to be just human and supportive. She showed me how to treat the
people I was training. … Dr. Swift was a formal person 99 percent of the time. You
knew that there was more to her, but you didn’t get a look at it very often. … She
did the mammography at the hospital and didn’t have a lot of time for other things.
But I knew that I could go to her and say, ‘Look, I’m in a conundrum with this particular
case. I just don’t know which way to go.’ As a radiologist, you want to be careful
not to give people reasons to do a tremendous amount of additional studies that don’t
go anywhere. On the other hand, you don’t want to overlook anything. Dr. Swift was
really good at that. I could count on her.” ”I met Marina in the mid to late seventies when I started as an attending at National
Naval Medical Center, as well as continuing my attending work at Walter Reed. She
was one of my first residents, and she impressed me from day one with the clarity
and completeness of her presentations. I was thrilled to learn that she was a fellow
PCOM graduate [one of 14 women in her class of 275]. … At some point after her residency
and after her first Navy assignment—she had a Navy health professions scholarship—Marina
decided to come over to the Army, for a variety of reasons. She was on staff at Walter
Reed. By then I had gone to the assignments branch, so I kept running into her and
seeing her progress. Things were not easy in those days, I’ll tell you quite frankly,
for a woman, particularly in cardiology, and there was skepticism about noninvasive
cardiology, which was her area. Cardiac ultrasound and all the imaging wasn’t nearly
as sophisticated then as it is today. She did very well, and
”I met Marina in the mid to late seventies when I started as an attending at National
Naval Medical Center, as well as continuing my attending work at Walter Reed. She
was one of my first residents, and she impressed me from day one with the clarity
and completeness of her presentations. I was thrilled to learn that she was a fellow
PCOM graduate [one of 14 women in her class of 275]. … At some point after her residency
and after her first Navy assignment—she had a Navy health professions scholarship—Marina
decided to come over to the Army, for a variety of reasons. She was on staff at Walter
Reed. By then I had gone to the assignments branch, so I kept running into her and
seeing her progress. Things were not easy in those days, I’ll tell you quite frankly,
for a woman, particularly in cardiology, and there was skepticism about noninvasive
cardiology, which was her area. Cardiac ultrasound and all the imaging wasn’t nearly
as sophisticated then as it is today. She did very well, and  “Courtney’s always been very engaging, very determined—laser-focused. You knew that
she was going to be successful, not because things were going to come easy for her
but because she was disciplined, thoughtful, and intentional about her future goals,
what her plan was. From that perspective, she always stood out to me. … Courtney was
fun, too. She never let anything get her down. She’s a strong personality who’s going
to fight for what she believes is right. She had her shares of ups and downs, but
you couldn’t keep her down. Some people may have a setback, and they allow that to
dictate where they go in life. Courtney’s reaction was to say: okay, let me figure
out a different way of achieving my goals. You take lemons, and you make lemonade.
… Courtney supported herself financially since a fairly young age. One summer she
was in a clinical research program at Memorial Sloan Kettering Cancer Center in New
York, which she described as a phenomenal experience. She was seeking not only to
enhance her clinical knowledge but also to earn income. I think it makes you a little
bit more compassionate when you understand the extra effort that it takes to be able
to survive and succeed when you have some things against you. … A few years ago, Courtney
started a primary care clinic, Fleur-De-Lis, in New Orleans, and she makes it a priority
to do community outreach. Now Fleur-De-Lis also has an aesthetics practice—skincare,
Botox, and fillers. Courtney had been interested in dermatology, and she was creative
about her professional path, keeping the focus on whole-person, preventative care.
That’s what I’ve seen in her from day one. It’s a special person that can say, I’m
not going to be sidetracked by these obstacles, because at the end of the day this
is where I want to be.”
“Courtney’s always been very engaging, very determined—laser-focused. You knew that
she was going to be successful, not because things were going to come easy for her
but because she was disciplined, thoughtful, and intentional about her future goals,
what her plan was. From that perspective, she always stood out to me. … Courtney was
fun, too. She never let anything get her down. She’s a strong personality who’s going
to fight for what she believes is right. She had her shares of ups and downs, but
you couldn’t keep her down. Some people may have a setback, and they allow that to
dictate where they go in life. Courtney’s reaction was to say: okay, let me figure
out a different way of achieving my goals. You take lemons, and you make lemonade.
… Courtney supported herself financially since a fairly young age. One summer she
was in a clinical research program at Memorial Sloan Kettering Cancer Center in New
York, which she described as a phenomenal experience. She was seeking not only to
enhance her clinical knowledge but also to earn income. I think it makes you a little
bit more compassionate when you understand the extra effort that it takes to be able
to survive and succeed when you have some things against you. … A few years ago, Courtney
started a primary care clinic, Fleur-De-Lis, in New Orleans, and she makes it a priority
to do community outreach. Now Fleur-De-Lis also has an aesthetics practice—skincare,
Botox, and fillers. Courtney had been interested in dermatology, and she was creative
about her professional path, keeping the focus on whole-person, preventative care.
That’s what I’ve seen in her from day one. It’s a special person that can say, I’m
not going to be sidetracked by these obstacles, because at the end of the day this
is where I want to be.” ”Dr. White was a family doctor who practiced osteopathic medicine in my hometown,
Lancaster City, Pennsylvania, for 50 years. My mom came to the United States when
she was eight years old, and Dr. White was her first doctor here. He ended up being
the primary doctor for three generations of my family. … He understood the struggle
of poverty and empathized with my grandma, who was raising three children in a new
city. No matter where you were, or the time of day, if you needed Dr. White, he was
there. He even did house calls. He didn’t care where you were from. He didn’t care
how much money you had or if you had insurance. … Later in life, Mom had some serious
back issues, and Dr. White was the first doctor to treat her with osteopathic manipulation.
She had very severe spinal herniations, and no one had ever tried this. I thought,
‘What’s going on?,’ and he explained it to me when I was a little girl. … He was very
proud of what he learned from PCOM. He had a PCOM poster in his office, and now his
daughter is going to give that poster to me. That’s a full circle moment. … When I
told him I wanted to be a doctor, he looked at me. Then he grabbed a little piece
of scrap paper, and he wrote something—I remember ‘biology, pre-medicine’—and he handed
it to me. He said, ‘Do this, and you’re going to be successful. And don’t let anyone
tell you no.’ And that stuck with me. … Not only was I a first-generation college
student, but now I’m a first-generation osteopathic medical student because of his
guidance and faith in me. He was always asking me, ‘How are those grades? If they’re
not an ace, I don’t want to know!’ He had a sense of humor. ‘An 89? That’s not good
enough! You’ve got to get a 90.’ … Dr. White used to tell patients to believe in themselves,
to advocate for themselves. He was a true osteopathic physician in that he saw beyond
the symptoms. He saw the whole person, and not just the person, but the family. And
not only the family, but the future for the family. That’s something I take very personally.
I plan to follow in Dr. White’s footsteps as a family doctor and look forward to serving
the same populations with such a giving heart as he did. Today, I am a mentor for
high schoolers and pre-meds, and in that way, I’m also honoring Dr. White’s memory.”
”Dr. White was a family doctor who practiced osteopathic medicine in my hometown,
Lancaster City, Pennsylvania, for 50 years. My mom came to the United States when
she was eight years old, and Dr. White was her first doctor here. He ended up being
the primary doctor for three generations of my family. … He understood the struggle
of poverty and empathized with my grandma, who was raising three children in a new
city. No matter where you were, or the time of day, if you needed Dr. White, he was
there. He even did house calls. He didn’t care where you were from. He didn’t care
how much money you had or if you had insurance. … Later in life, Mom had some serious
back issues, and Dr. White was the first doctor to treat her with osteopathic manipulation.
She had very severe spinal herniations, and no one had ever tried this. I thought,
‘What’s going on?,’ and he explained it to me when I was a little girl. … He was very
proud of what he learned from PCOM. He had a PCOM poster in his office, and now his
daughter is going to give that poster to me. That’s a full circle moment. … When I
told him I wanted to be a doctor, he looked at me. Then he grabbed a little piece
of scrap paper, and he wrote something—I remember ‘biology, pre-medicine’—and he handed
it to me. He said, ‘Do this, and you’re going to be successful. And don’t let anyone
tell you no.’ And that stuck with me. … Not only was I a first-generation college
student, but now I’m a first-generation osteopathic medical student because of his
guidance and faith in me. He was always asking me, ‘How are those grades? If they’re
not an ace, I don’t want to know!’ He had a sense of humor. ‘An 89? That’s not good
enough! You’ve got to get a 90.’ … Dr. White used to tell patients to believe in themselves,
to advocate for themselves. He was a true osteopathic physician in that he saw beyond
the symptoms. He saw the whole person, and not just the person, but the family. And
not only the family, but the future for the family. That’s something I take very personally.
I plan to follow in Dr. White’s footsteps as a family doctor and look forward to serving
the same populations with such a giving heart as he did. Today, I am a mentor for
high schoolers and pre-meds, and in that way, I’m also honoring Dr. White’s memory.” On May 18, 1896, the U.S. Supreme Court issued its Plessy v. Ferguson ruling, which upheld the constitutionality of racial segregation laws within the
“separate but equal” doctrine. That was the world Edna D. Kennedy had been born into
just five weeks prior. As an African American, she would face challenges in a society
that did not offer separate but equal opportunities into the medical profession. Not
only would her race limit her access to medical schools; so, too, would her gender.
Despite the odds, this native Philadelphian—known as Edna K. Williams, DO, throughout
her career—would follow in the footsteps of
On May 18, 1896, the U.S. Supreme Court issued its Plessy v. Ferguson ruling, which upheld the constitutionality of racial segregation laws within the
“separate but equal” doctrine. That was the world Edna D. Kennedy had been born into
just five weeks prior. As an African American, she would face challenges in a society
that did not offer separate but equal opportunities into the medical profession. Not
only would her race limit her access to medical schools; so, too, would her gender.
Despite the odds, this native Philadelphian—known as Edna K. Williams, DO, throughout
her career—would follow in the footsteps of  ”Daniel Wisely was a very special gentleman. He came into a profession that was often,
and still sometimes is, stigmatized as being rude or blunt. But he was so open, sincere,
caring. … Yes, you had to work hard. You had to always be at your best. You had to
bring a hundred percent, all the time. But he also recognized the sacrifices of the
profession to your personal life, to your family. … I can remember him walking around
the hospital, and something might be a bit ajar, and he’d take a moment to help out
housekeeping, or pause while a nurse was with a patient rather than come in with a
bluster. … When I was a resident in surgery, there weren’t that many of us, and you
might be unable to get any time off. He’d say, ‘I’ll cover for you. I got this. You
need to go home; you’ve been on for three weeks in a row.’… He was a consummate surgeon.
I don’t think I ever saw him falter or sweat. He called himself a little country doctor,
but his skills were just phenomenal. He had these big hands but such a subtle touch.
… He was proud of all his residents and graduates, and of their successes over time.
He had an ability to see not only people’s potential, but to take the next step of
saying, ‘What can I do to help?’ … He wouldn’t let you in real close to him personally;
he was a quiet and private man. But you knew he really cared. … He always made the
time when the time was necessary. He just seemed to know. He had a great skillset
of people understanding—listening, interpreting, getting to the bottom of something,
not just reacting in a moment in time. Today, you can read all the books on management,
but this was another era. How did he do it? … If I’m going into a difficult situation,
whether to talk to a family about a loved one who is maybe going to pass, or to have
a difficult conversation about something at work, I often think about the demeanor
that he drew upon. And so it’s more than ‘What would Dan do?’—of course, we never
would have called him Dan!—but ‘Without losing himself, how did he find the space
to give everyone their due, their necessary attention? What was the essence?’”
”Daniel Wisely was a very special gentleman. He came into a profession that was often,
and still sometimes is, stigmatized as being rude or blunt. But he was so open, sincere,
caring. … Yes, you had to work hard. You had to always be at your best. You had to
bring a hundred percent, all the time. But he also recognized the sacrifices of the
profession to your personal life, to your family. … I can remember him walking around
the hospital, and something might be a bit ajar, and he’d take a moment to help out
housekeeping, or pause while a nurse was with a patient rather than come in with a
bluster. … When I was a resident in surgery, there weren’t that many of us, and you
might be unable to get any time off. He’d say, ‘I’ll cover for you. I got this. You
need to go home; you’ve been on for three weeks in a row.’… He was a consummate surgeon.
I don’t think I ever saw him falter or sweat. He called himself a little country doctor,
but his skills were just phenomenal. He had these big hands but such a subtle touch.
… He was proud of all his residents and graduates, and of their successes over time.
He had an ability to see not only people’s potential, but to take the next step of
saying, ‘What can I do to help?’ … He wouldn’t let you in real close to him personally;
he was a quiet and private man. But you knew he really cared. … He always made the
time when the time was necessary. He just seemed to know. He had a great skillset
of people understanding—listening, interpreting, getting to the bottom of something,
not just reacting in a moment in time. Today, you can read all the books on management,
but this was another era. How did he do it? … If I’m going into a difficult situation,
whether to talk to a family about a loved one who is maybe going to pass, or to have
a difficult conversation about something at work, I often think about the demeanor
that he drew upon. And so it’s more than ‘What would Dan do?’—of course, we never
would have called him Dan!—but ‘Without losing himself, how did he find the space
to give everyone their due, their necessary attention? What was the essence?’” ”Dr. Young was a large figure at the podium, and he took up most of the front of the
classroom with his personality. He obviously was teaching surgery, but at same time
he seamlessly wove together the different disciplines to make for one medical philosophy.
That impressed me quite a bit as a second-year DO student. … When I was on his service,
what struck me was that he knew his patients by their first names and had treated
them multiple times. That’s because he not only had a surgical practice, he had a
family medicine practice—he ran both together. So he wasn’t just someone a patient
encountered at the last moment of a critical phase of their disease. … I’ve been involved
in surgery now for almost 45 years, and I have never seen anybody have dual practices.
More importantly, I have never seen anybody have their surgical residents manage both.
I think the residents came to appreciate that skill later, as they went into their
own practices. … I was the chairman of the
”Dr. Young was a large figure at the podium, and he took up most of the front of the
classroom with his personality. He obviously was teaching surgery, but at same time
he seamlessly wove together the different disciplines to make for one medical philosophy.
That impressed me quite a bit as a second-year DO student. … When I was on his service,
what struck me was that he knew his patients by their first names and had treated
them multiple times. That’s because he not only had a surgical practice, he had a
family medicine practice—he ran both together. So he wasn’t just someone a patient
encountered at the last moment of a critical phase of their disease. … I’ve been involved
in surgery now for almost 45 years, and I have never seen anybody have dual practices.
More importantly, I have never seen anybody have their surgical residents manage both.
I think the residents came to appreciate that skill later, as they went into their
own practices. … I was the chairman of the  “When I first arrived at PCOM in 2015, I met with each member of the Board of Trustees
to hear their perspectives on the College. It took a fair bit of cajoling for Dr.
Zedeck to agree to meet with me, but what was supposed to be a one-hour lunch turned
into a three-hour meeting of kindred spirits. My absolute favorite moment was when
he explained to me that ‘in order for alumni to be disgruntled, they have to first
be gruntled,’ and Dr. Zedeck wanted to be gruntled again. From that moment, Dr. Zedeck
has been a mentor, guide, critic and friend to me, never one to hesitate to share
his ideas and speak his mind. … Dr. Zedeck’s creativity and practicality were forged
during his career as a pharmacist, then as an osteopathic family medicine physician,
and finally as the founder of several community banks in South Florida. We talked
at length at that first lunch, and in multiple conversations thereafter, about how
frustrated we got when we saw an idea, recognized the positive impact it could have,
but couldn’t get traction. I believe this is what cemented our bond: Dr. Zedeck had
an idea, I recognized the positive impact of that idea, and together, we made it happen.
… Incorporating humanities into medical education? Dr. Zedeck funded a lecture series
for just that purpose, and I made certain that three lectures were held each year.
“When I first arrived at PCOM in 2015, I met with each member of the Board of Trustees
to hear their perspectives on the College. It took a fair bit of cajoling for Dr.
Zedeck to agree to meet with me, but what was supposed to be a one-hour lunch turned
into a three-hour meeting of kindred spirits. My absolute favorite moment was when
he explained to me that ‘in order for alumni to be disgruntled, they have to first
be gruntled,’ and Dr. Zedeck wanted to be gruntled again. From that moment, Dr. Zedeck
has been a mentor, guide, critic and friend to me, never one to hesitate to share
his ideas and speak his mind. … Dr. Zedeck’s creativity and practicality were forged
during his career as a pharmacist, then as an osteopathic family medicine physician,
and finally as the founder of several community banks in South Florida. We talked
at length at that first lunch, and in multiple conversations thereafter, about how
frustrated we got when we saw an idea, recognized the positive impact it could have,
but couldn’t get traction. I believe this is what cemented our bond: Dr. Zedeck had
an idea, I recognized the positive impact of that idea, and together, we made it happen.
… Incorporating humanities into medical education? Dr. Zedeck funded a lecture series
for just that purpose, and I made certain that three lectures were held each year.
